/ Company
/ Company
/ Company
Zelis
Zelis
Zelis
/ Role
/ Role
/ Role
Sr. UX Designer
Sr. UX Designer
Sr. UX Designer
/ Date
/ Date
/ Date
2021-2024
2021-2024
2021-2024
medical
medical
medical
medical
Price
Price
Price
Price
Transparency
Transparency
Transparency
Transparency
[2]
[2]
[2]
/ About the project
/ About the project
/ About the project
A new law required healthcare providers and insurers to publish their prices for procedures. We built a tool to help patients make informed financial decisions using this data and guided the unprepared healthcare industry to building patient-centric solutions.
A new law required healthcare providers and insurers to publish their prices for procedures. We built a tool to help patients make informed financial decisions using this data and guided the unprepared healthcare industry to building patient-centric solutions.
A new law required healthcare providers and insurers to publish their prices for procedures. We built a tool to help patients make informed financial decisions using this data and guided the unprepared healthcare industry to building patient-centric solutions.
[Part 1]
price transparency
for patients
price transparency
for patients
price transparency
for patients
/ Price transparency
/ Price transparency
/ Price transparency
In 2020, the Transparency in Coverage bill was passed, requiring providers and health plans to publish their negotiated rates of all medical services.
In 2020, the Transparency in Coverage bill was passed, requiring providers and health plans to publish their negotiated rates of all medical services.
In 2020, the Transparency in Coverage bill was passed, requiring providers and health plans to publish their negotiated rates of all medical services.
/ Provider Directory
/ Provider Directory
/ Provider Directory
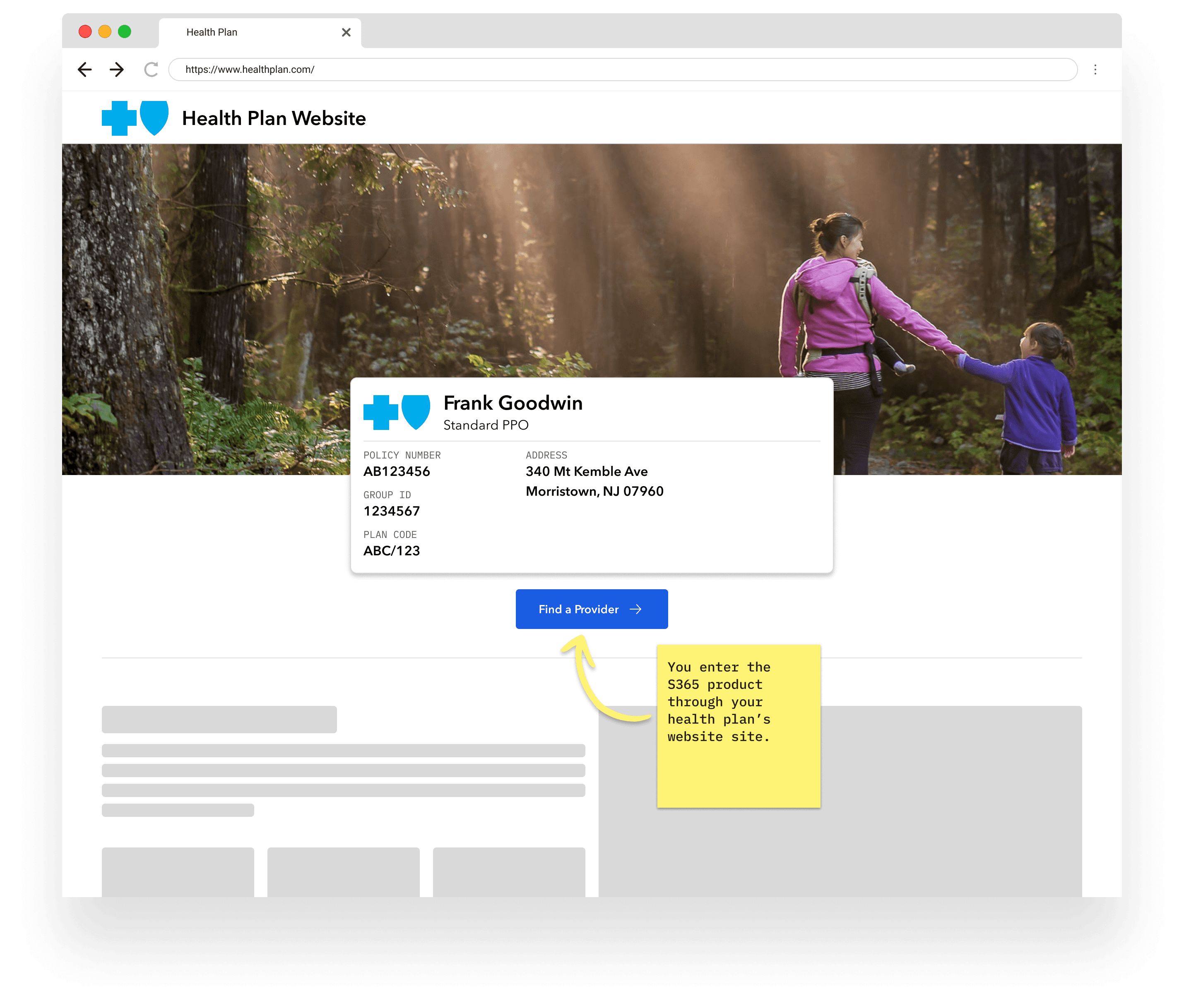
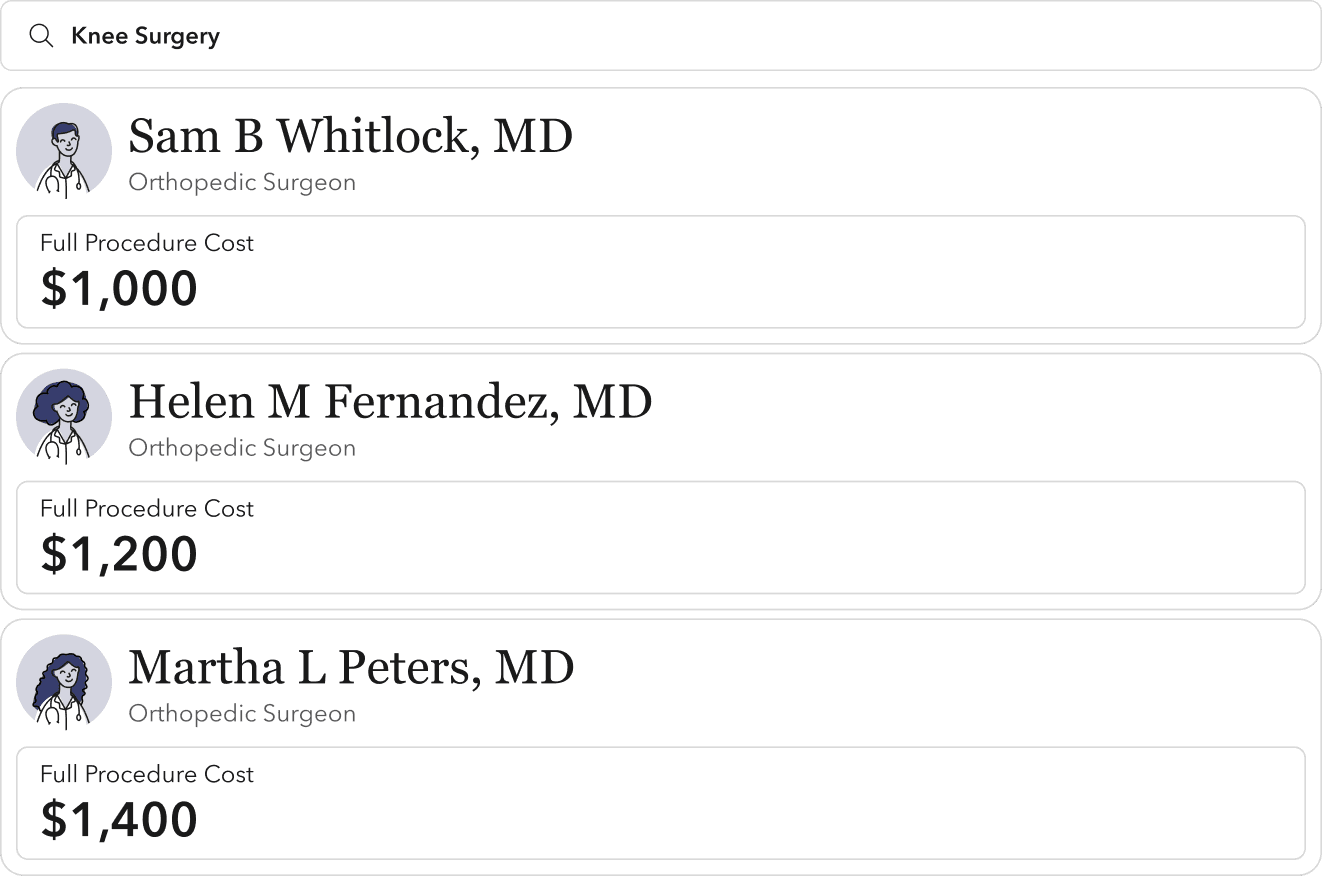
The Sapphire365 product is a procedure and provider directory, white-labeled for health insurance sites to help their members find in-network care. This is where we started.
The Sapphire365 product is a procedure and provider directory, white-labeled for health insurance sites to help their members find in-network care. This is where we started.
The Sapphire365 product is a procedure and provider directory, white-labeled for health insurance sites to help their members find in-network care. This is where we started.
/ Healthplan Clients
/ Healthplan Clients
/ Annual Users
/ Annual Users
M+
M+
M+
M+
/ Annual Searches
/ Annual Searches
M+
M+
M+
M+
/ Procedure Cost
/ Procedure Cost
/ Procedure Cost
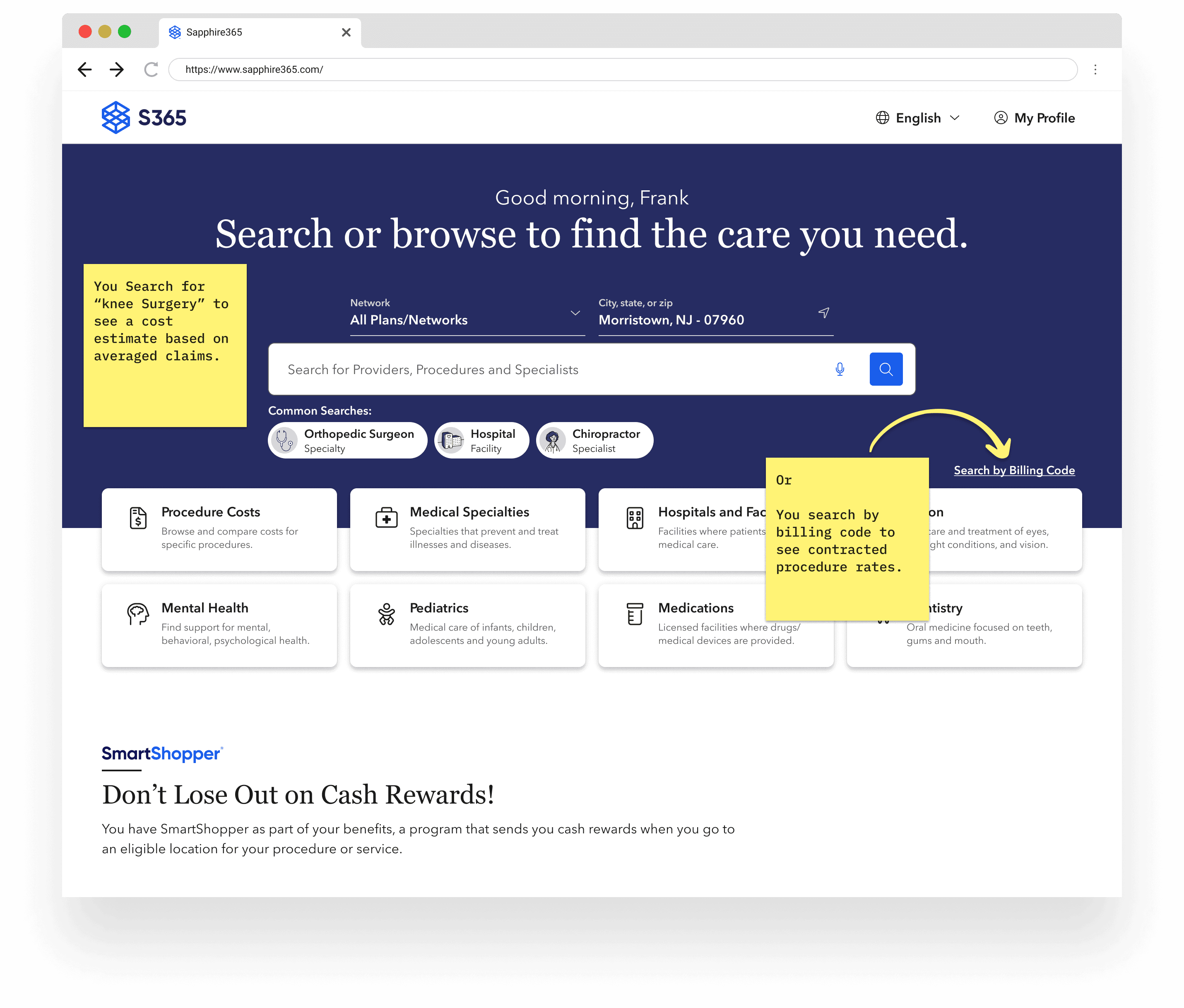
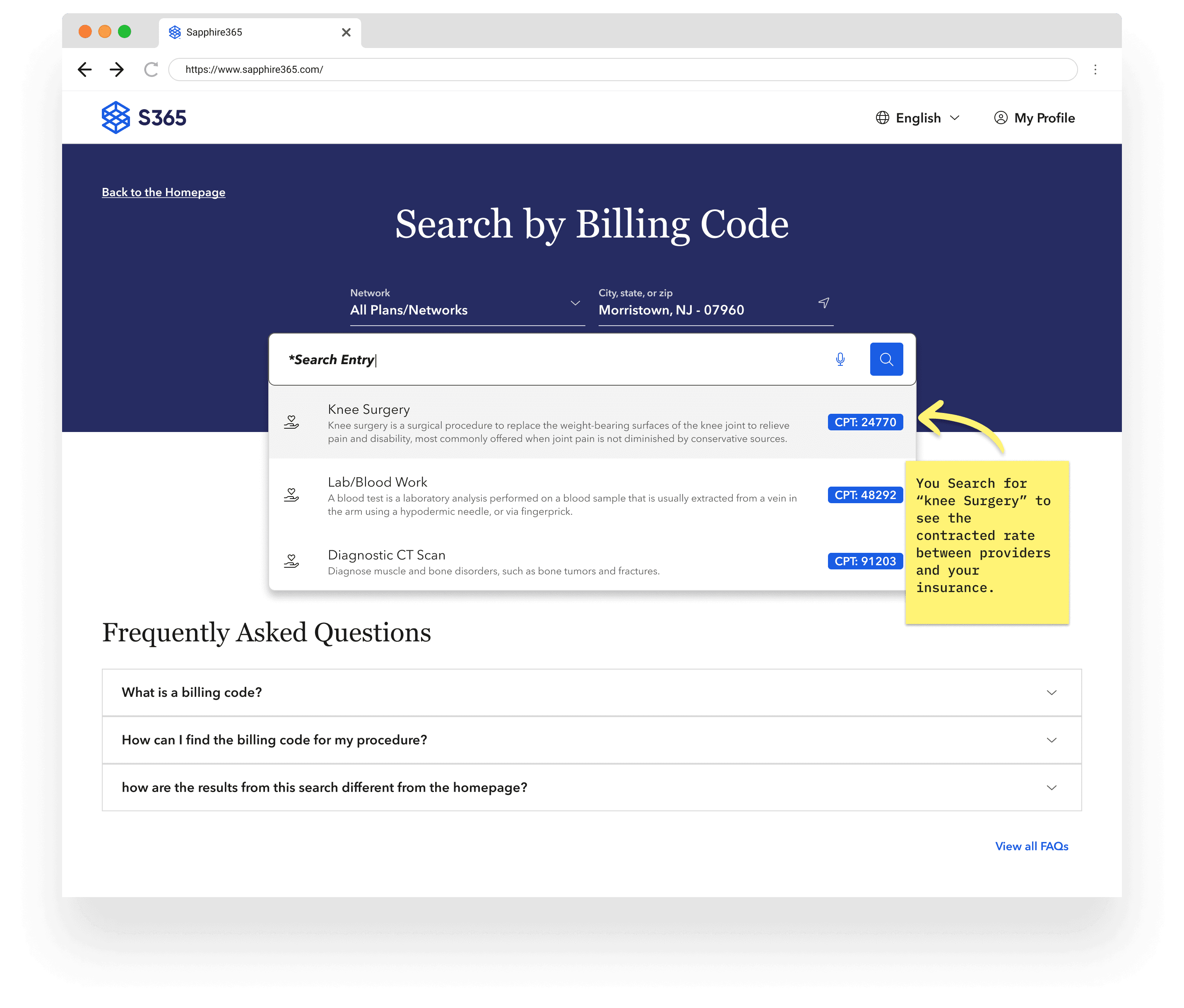
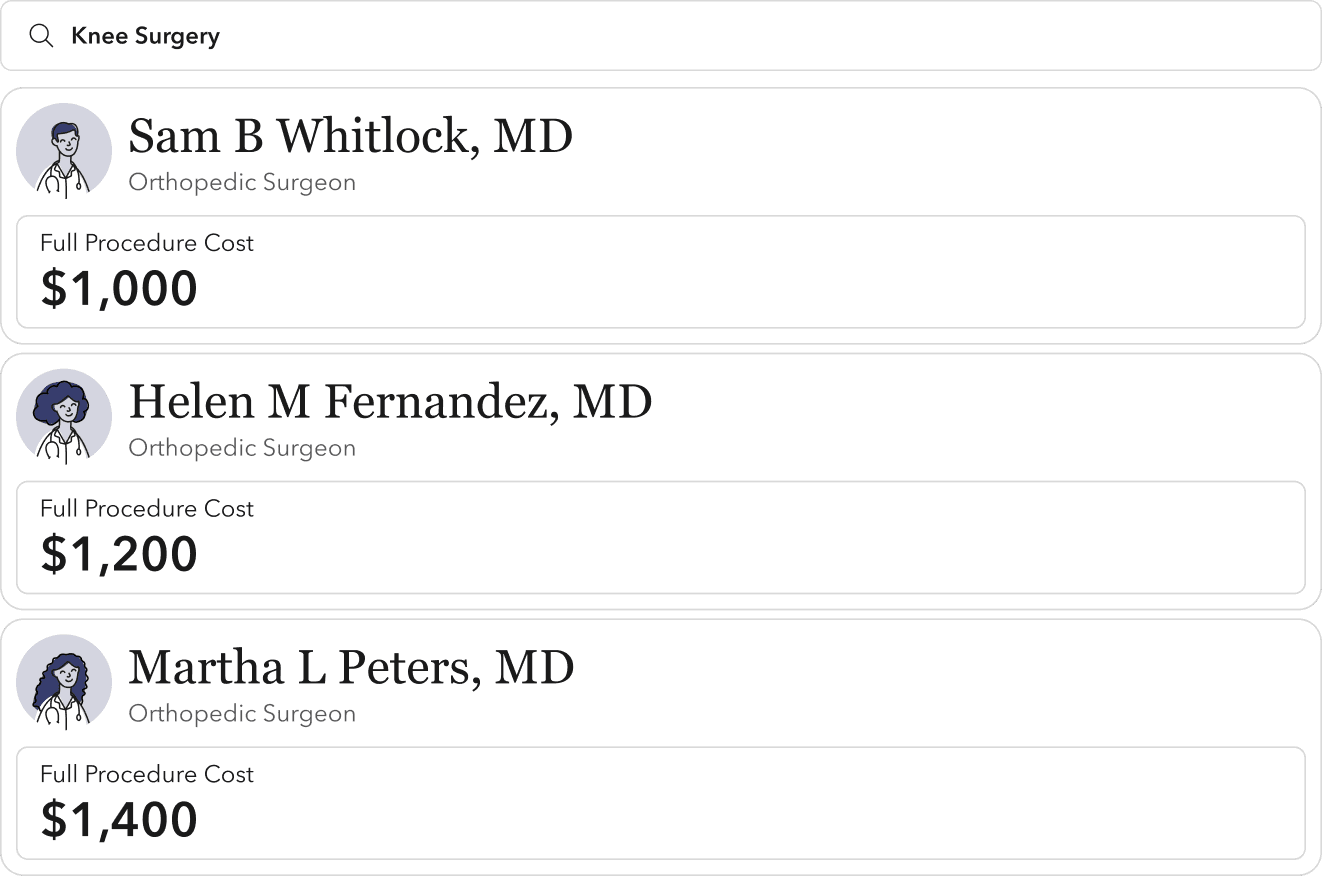
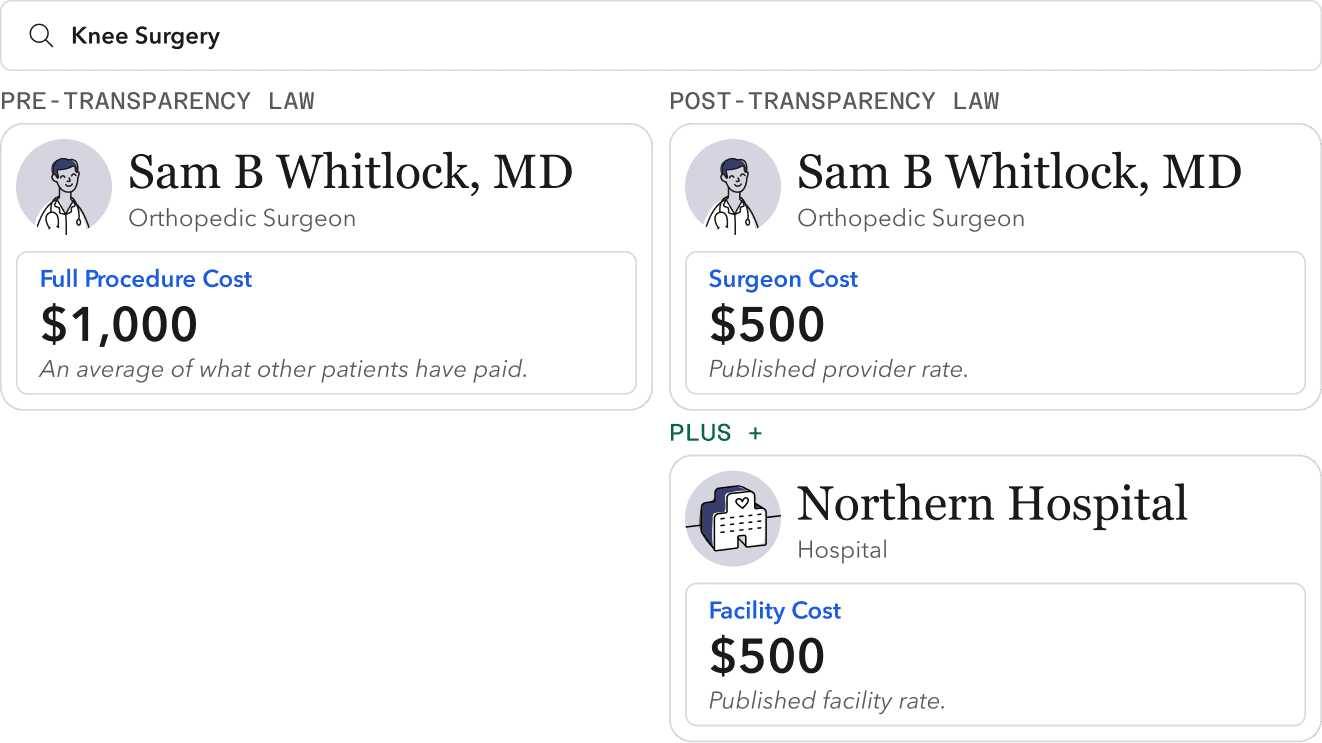
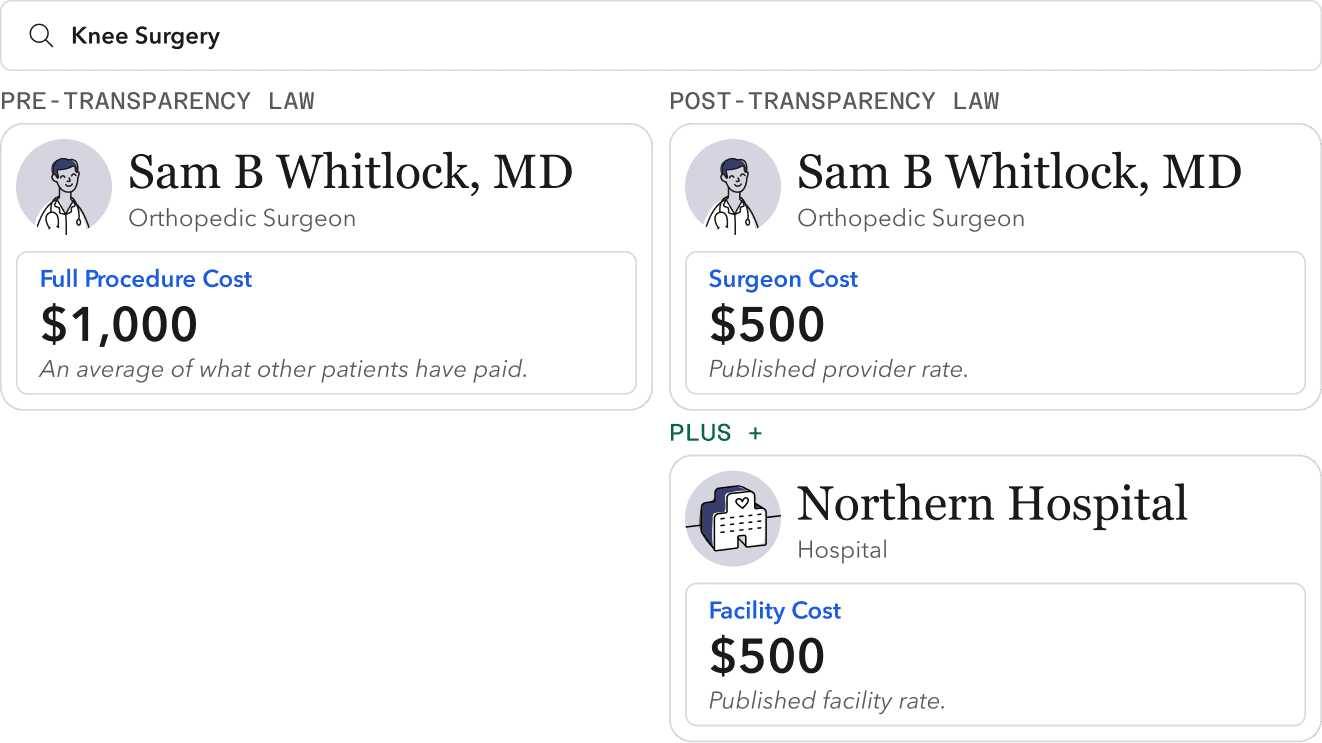
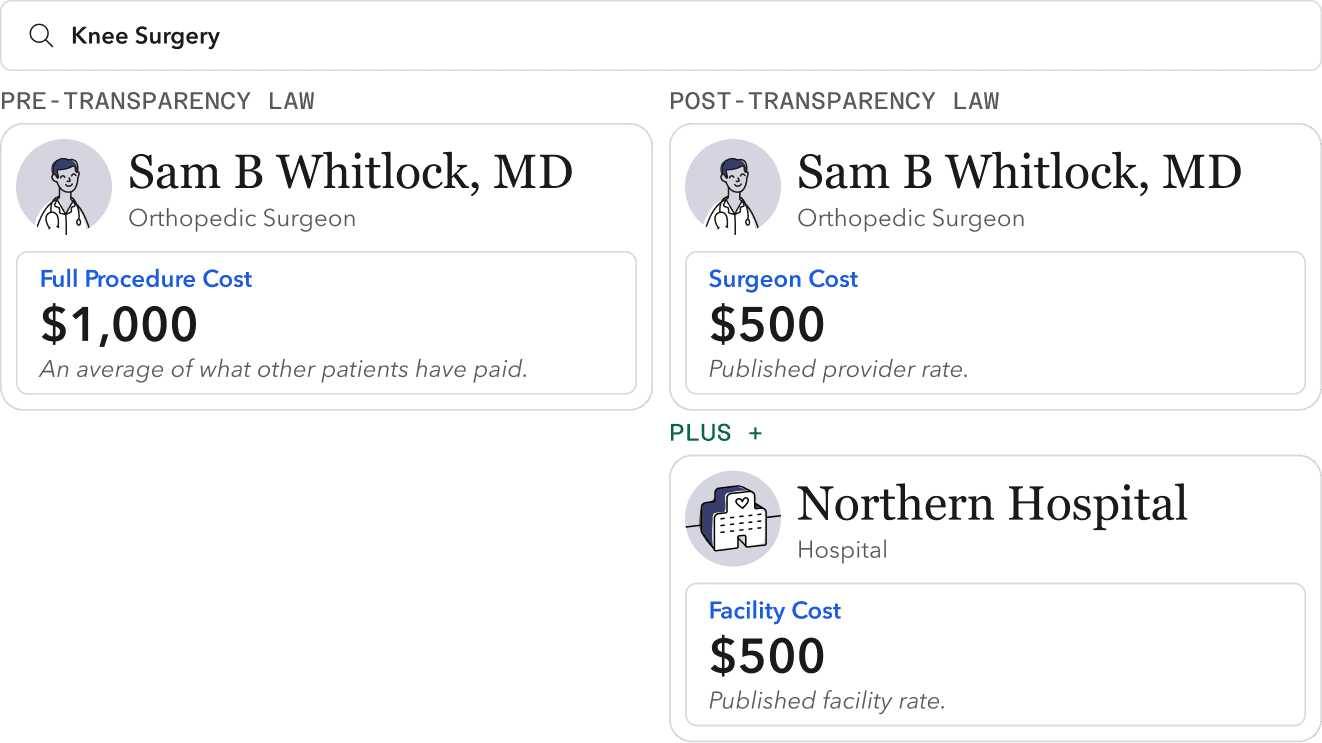
To date, medical cost estimates have been based on averaged patient claims. Which typically meant you could get a zoomed-out estimate of a full procedure cost.
With the new procedure price data, we can now view a detailed list of billed services for a specific procedure. These individual service costs are what the mandate requires to be published and searchable (not the full procedure cost.)
To date, medical cost estimates have been based on averaged patient claims. Which typically meant you could get a zoomed-out estimate of a full procedure cost.
With the new procedure price data, we can now view a detailed list of billed services for a specific procedure. These individual service costs are what the mandate requires to be published and searchable (not the full procedure cost.)
To date, medical cost estimates have been based on averaged patient claims. Which typically meant you could get a zoomed-out estimate of a full procedure cost.
With the new procedure price data, we can now view a detailed list of billed services for a specific procedure. These individual service costs are what the mandate requires to be published and searchable (not the full procedure cost.)
/ Unpacking the bill
/ Unpacking the bill
/ Unpacking the bill
In collaboration with our clients, legal teams, engineers, and government officials, we decoded the bill and formulated a two-year product roadmap aimed at a compliant and usable solution.
This included product requirements and a data infrastructure and augmentation strategy.
In collaboration with our clients, legal teams, engineers, and government officials, we decoded the bill and formulated a two-year product roadmap aimed at a compliant and usable solution.
This included co-informed product requirements and data infrastructure/augmentation strategy.
In collaboration with our clients, legal teams, engineers, and government officials, we decoded the bill and formulated a two-year product roadmap aimed at a compliant and usable solution.
This included co-informed product requirements and data infrastructure/augmentation strategy.
/ Healthcare Literacy
/ Healthcare Literacy
/ Healthcare Literacy
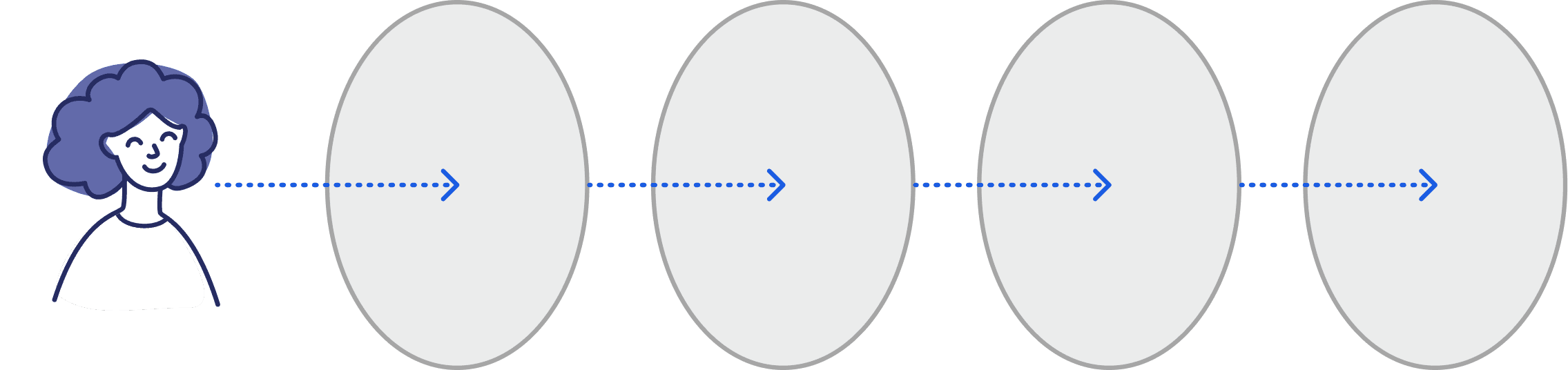
The fundamental insight we gained from our behavioral interviews is that the barrier to understanding healthcare is extremely high.
For users to confidently understand procedure costs, we needed to provide them with the right information at the right moment in their journey.
The fundamental insight we gained from running over 50 behavioral interviews is that the barrier to understanding healthcare is too high.
For users to comprehend procedure costs, we'd need to meet them with the right information at the right moment in their journey.
The fundamental insight we gained from running over 50 behavioral interviews is that the barrier to understanding healthcare is too high.
For users to comprehend procedure costs, we'd need to meet them with the right information at the right moment in their journey.
Medical Services
Medical Services
Medical Services
Insurance OPERATIONS
Insurance OPERATIONS
Insurance OPERATIONS
Coverage & Benefits
Coverage & Benefits
Coverage & Benefits
Cost information
Cost information
Cost information
/ Solution Strategy
/ Solution Strategy
/ Solution Strategy
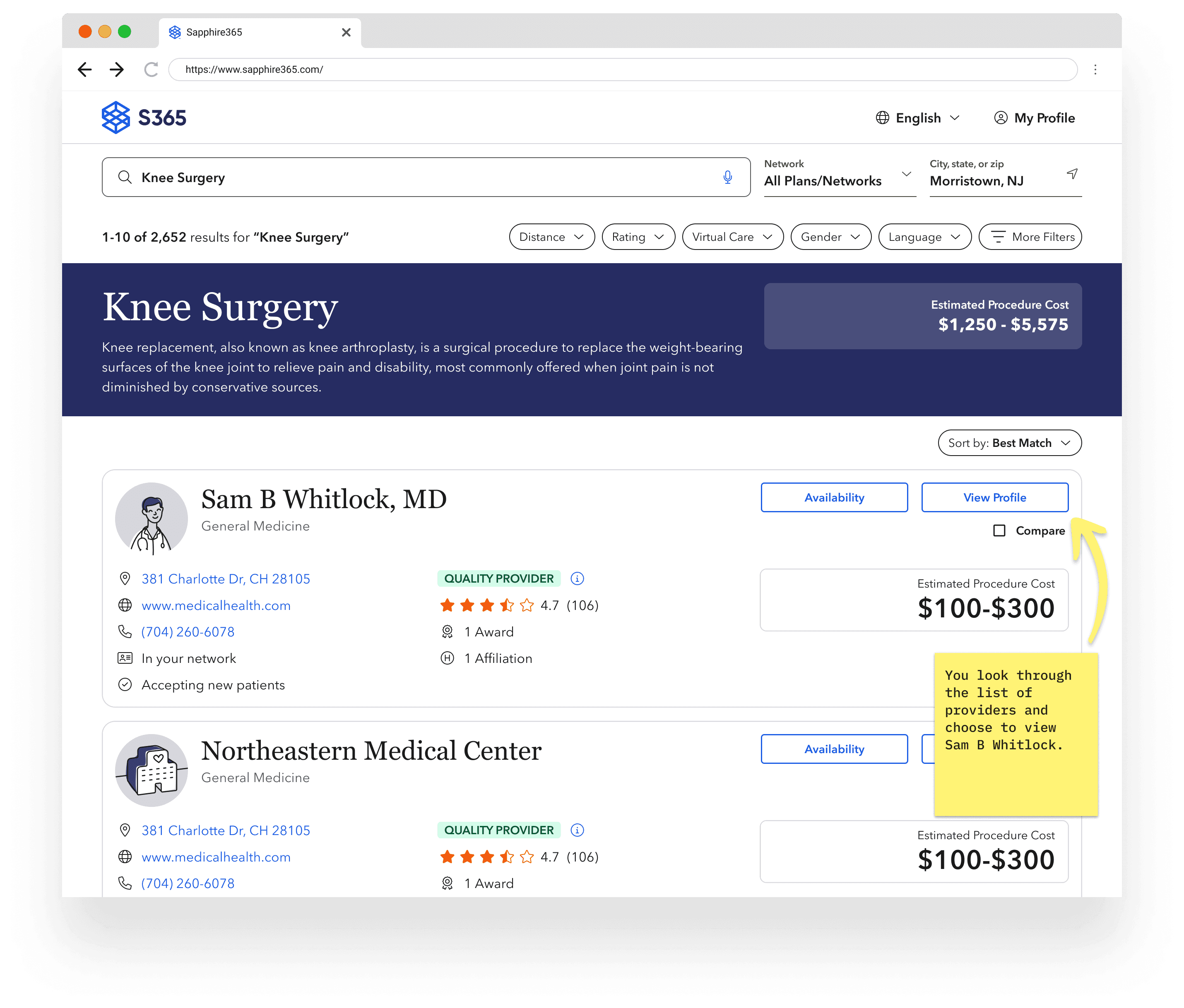
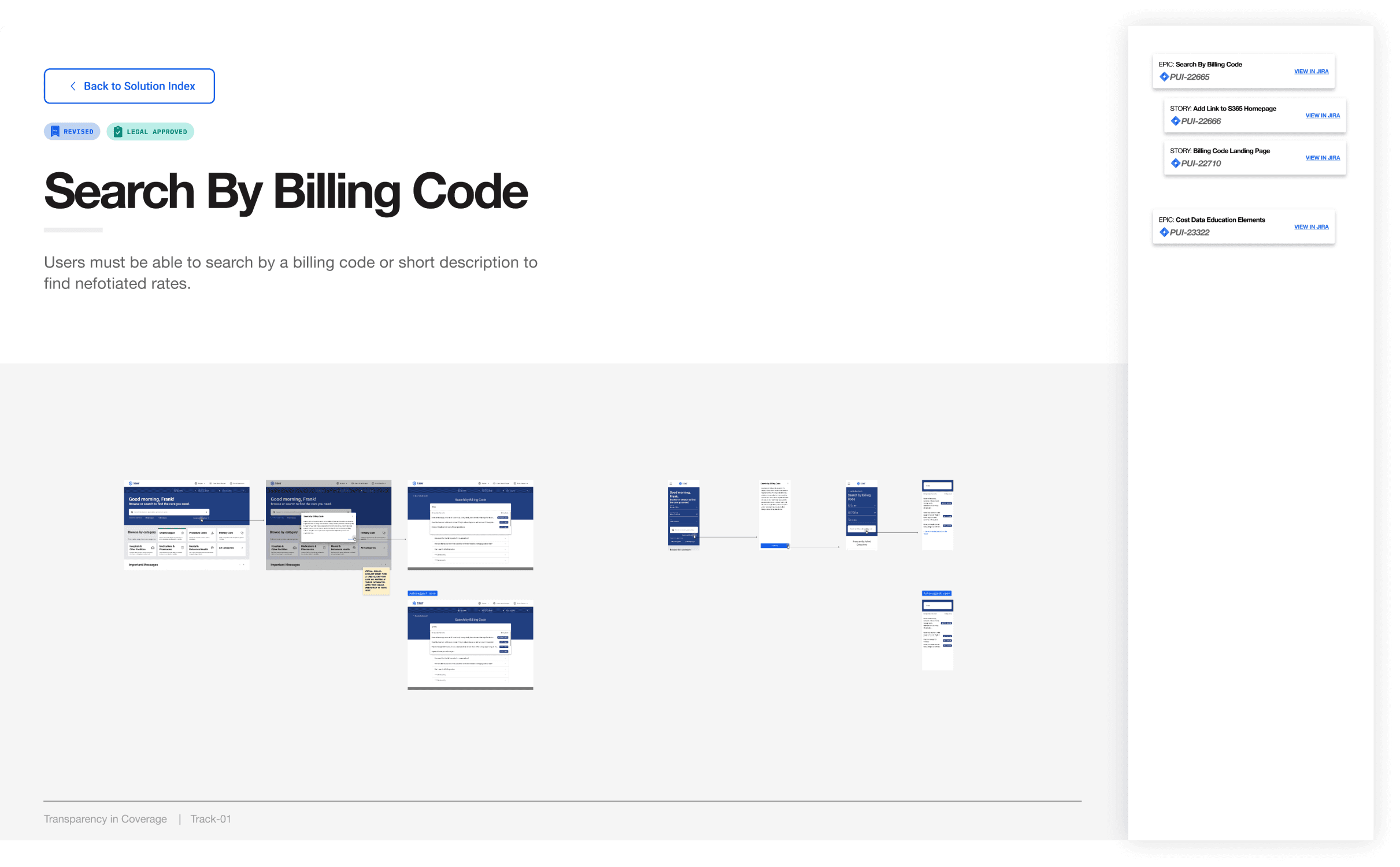
Applying user insights to opportunities along a care journey helped identify high-impact solution spaces and clarify the elements of the legislation that would not add value to users.
We ultimately focused on search result pages where users are analyzing multiple providers and provider profiles where they're seeing detailed cost information.
Applying user insights to opportunities along a care journey helped identify high-impact solution spaces and clarify the elements of the legislation that would not add value to users.
We ultimately focused on search result pages where users are analyzing multiple providers and provider profiles where they're seeing detailed cost information.
Applying user insights to opportunities along a care journey helped identify high-impact solution spaces and clarify the elements of the legislation that would not add value to users.
We ultimately focused on search result pages where users are analyzing multiple providers and provider profiles where they're seeing detailed cost information.
/ Data utility
/ Data utility
/ Data utility
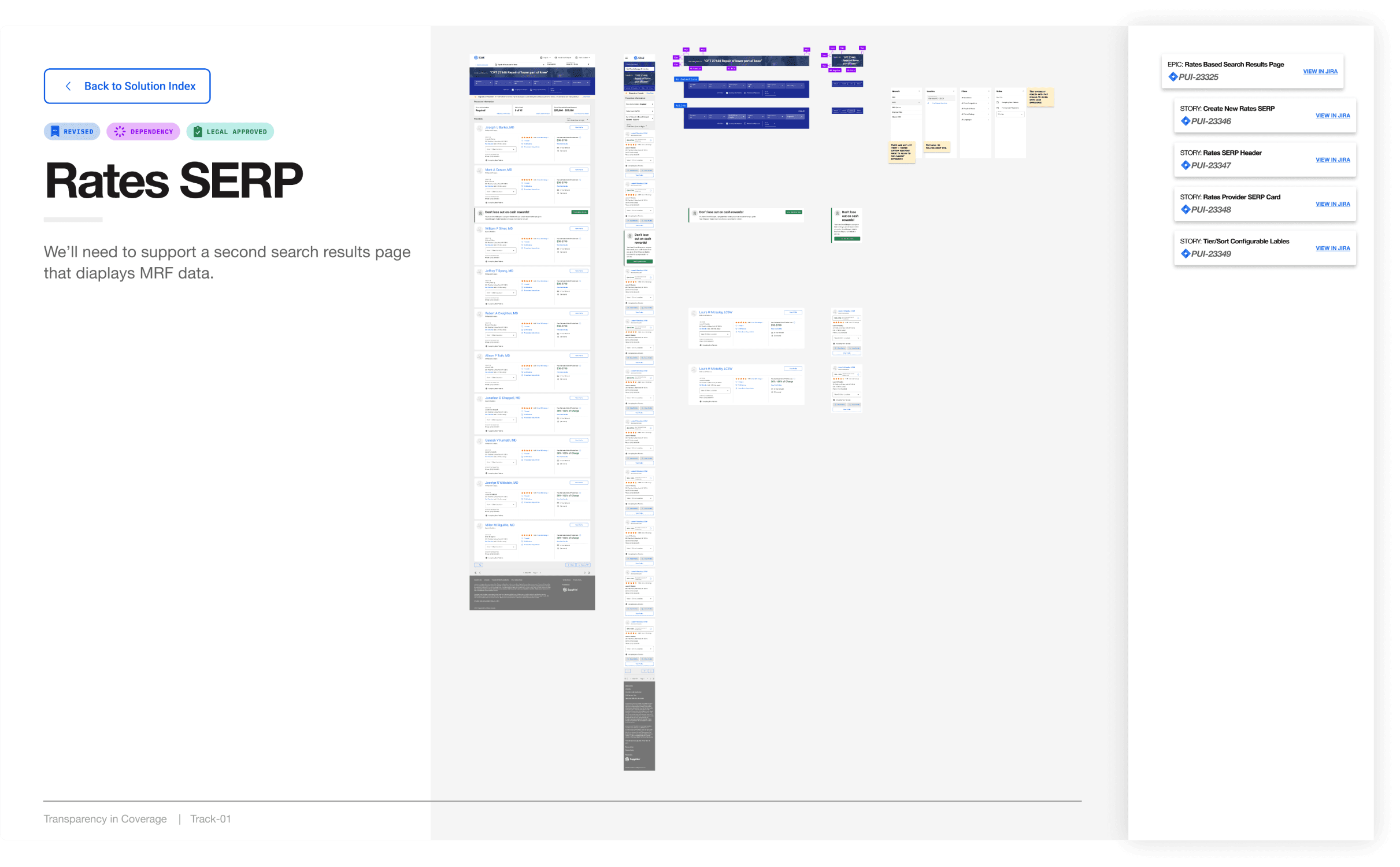
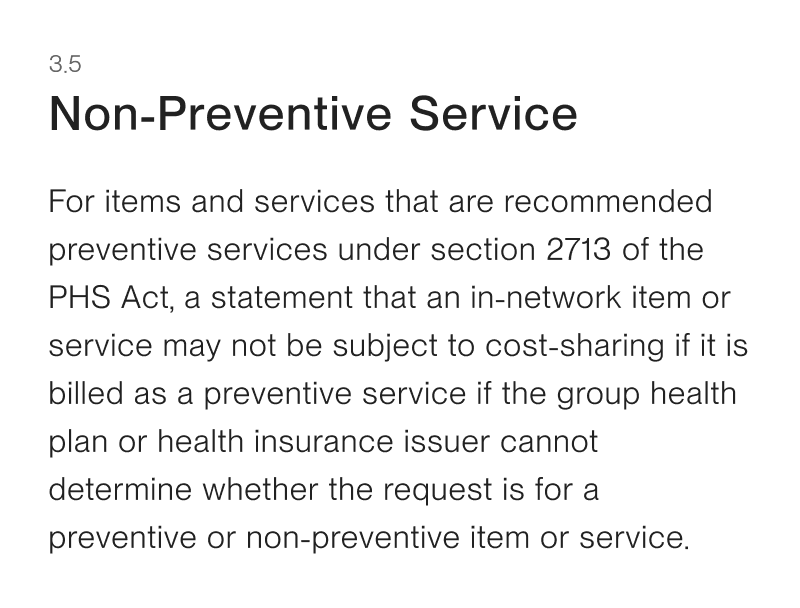
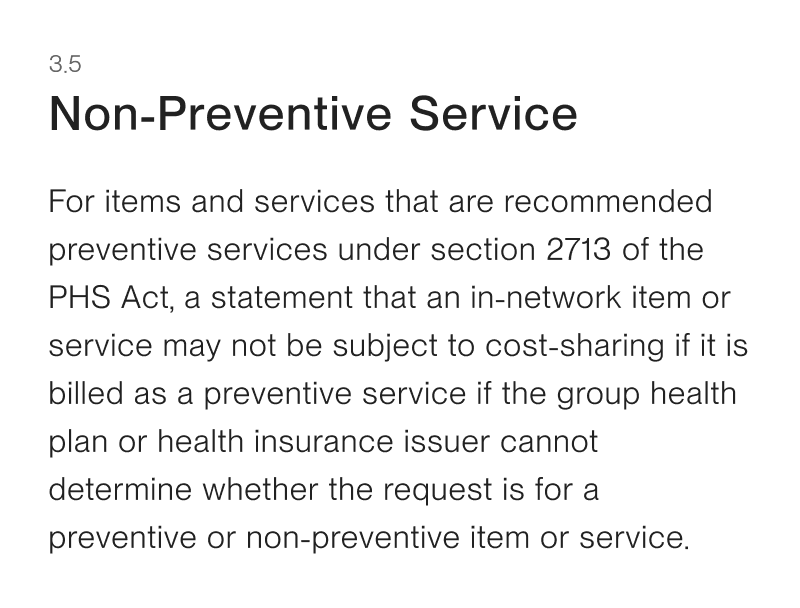
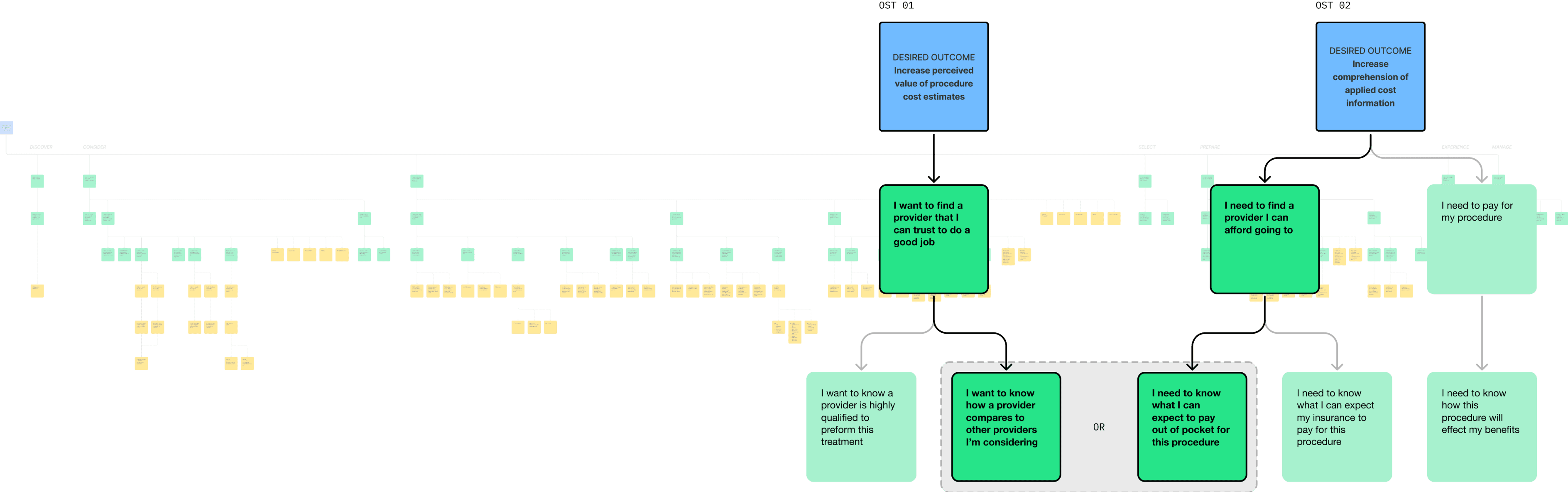
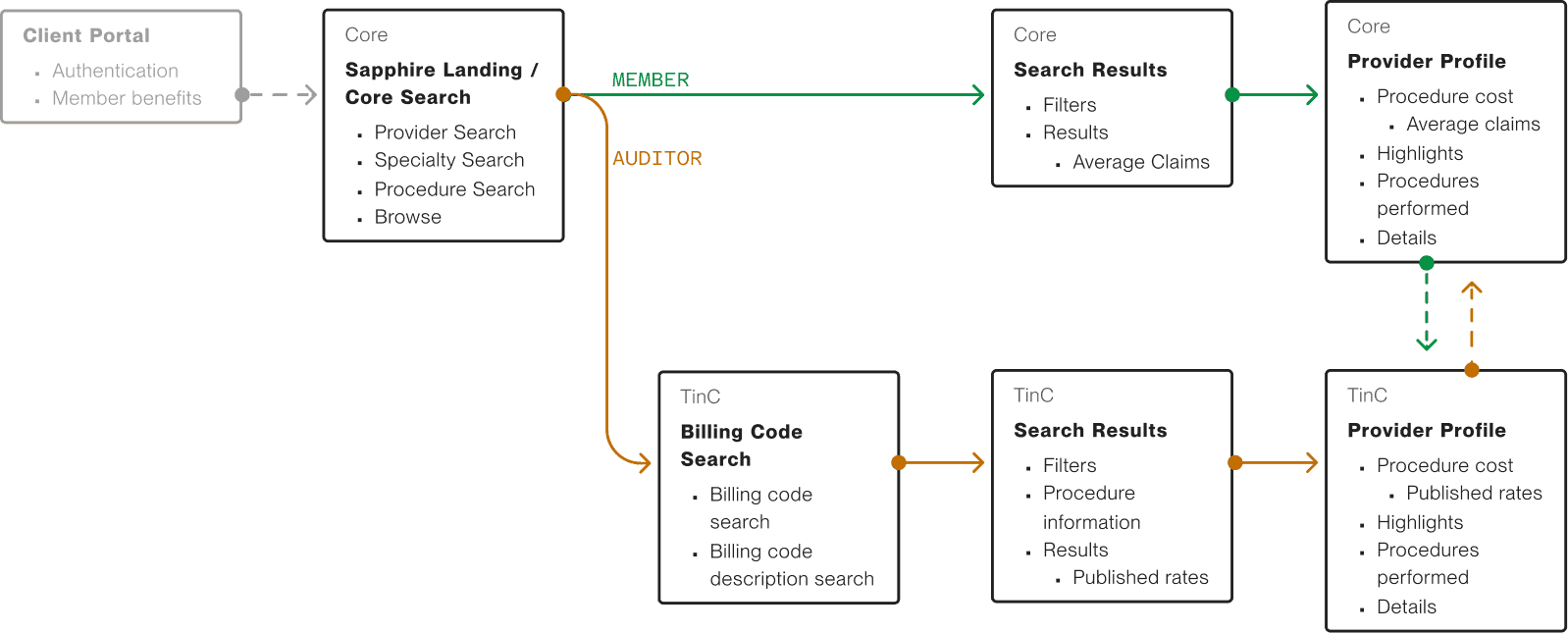
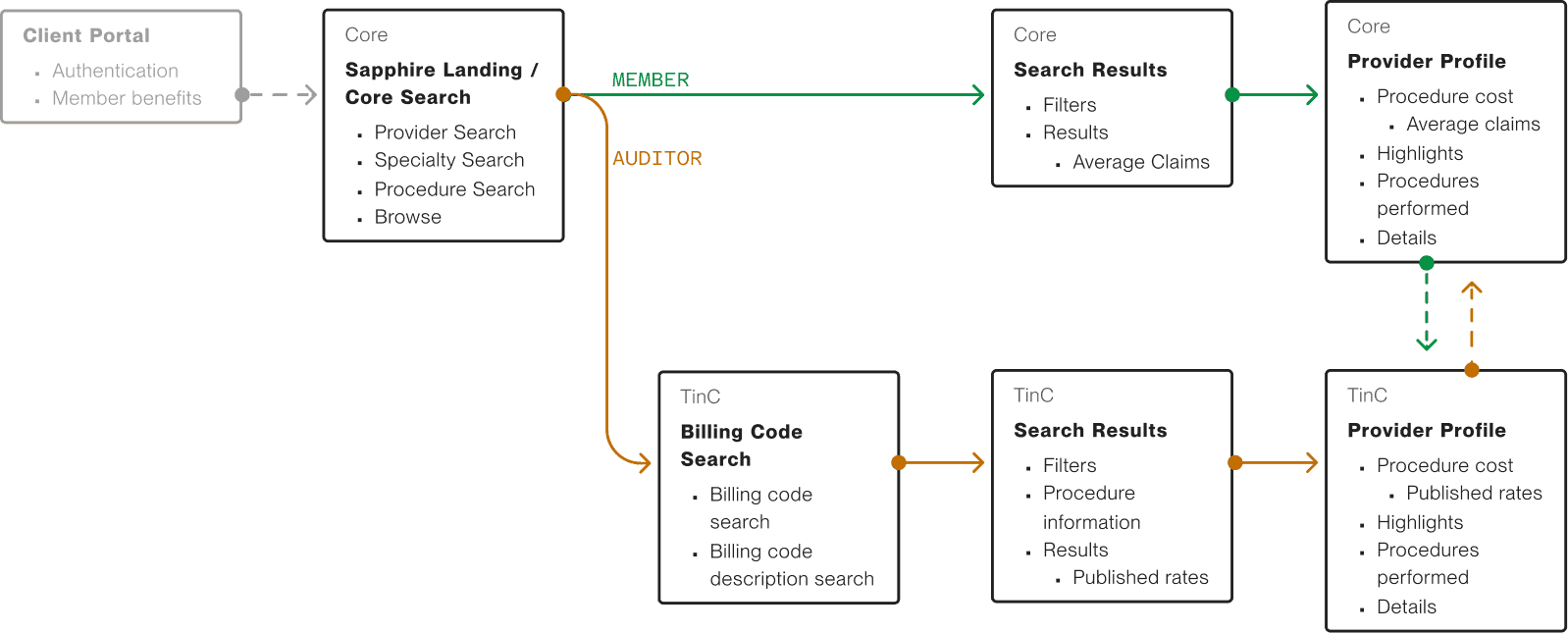
We leveraged the new data in ways that strengthened the existing member journey of finding care. We also developed a secondary flow for what we determined were compliance-only solutions, tailoring it for health insurance experts and auditors.
We leveraged the new data in ways that strengthened the existing member journey of finding care. We also developed a secondary flow for what we determined were compliance-only solutions, tailoring it for health insurance experts and auditors.
We leveraged the new data in ways that strengthened the existing member journey of finding care. We also developed a secondary flow for what we determined were compliance-only solutions, tailoring it for health insurance experts and auditors.
/ [Auditor] Flow
Drag →
Drag →
Drag →
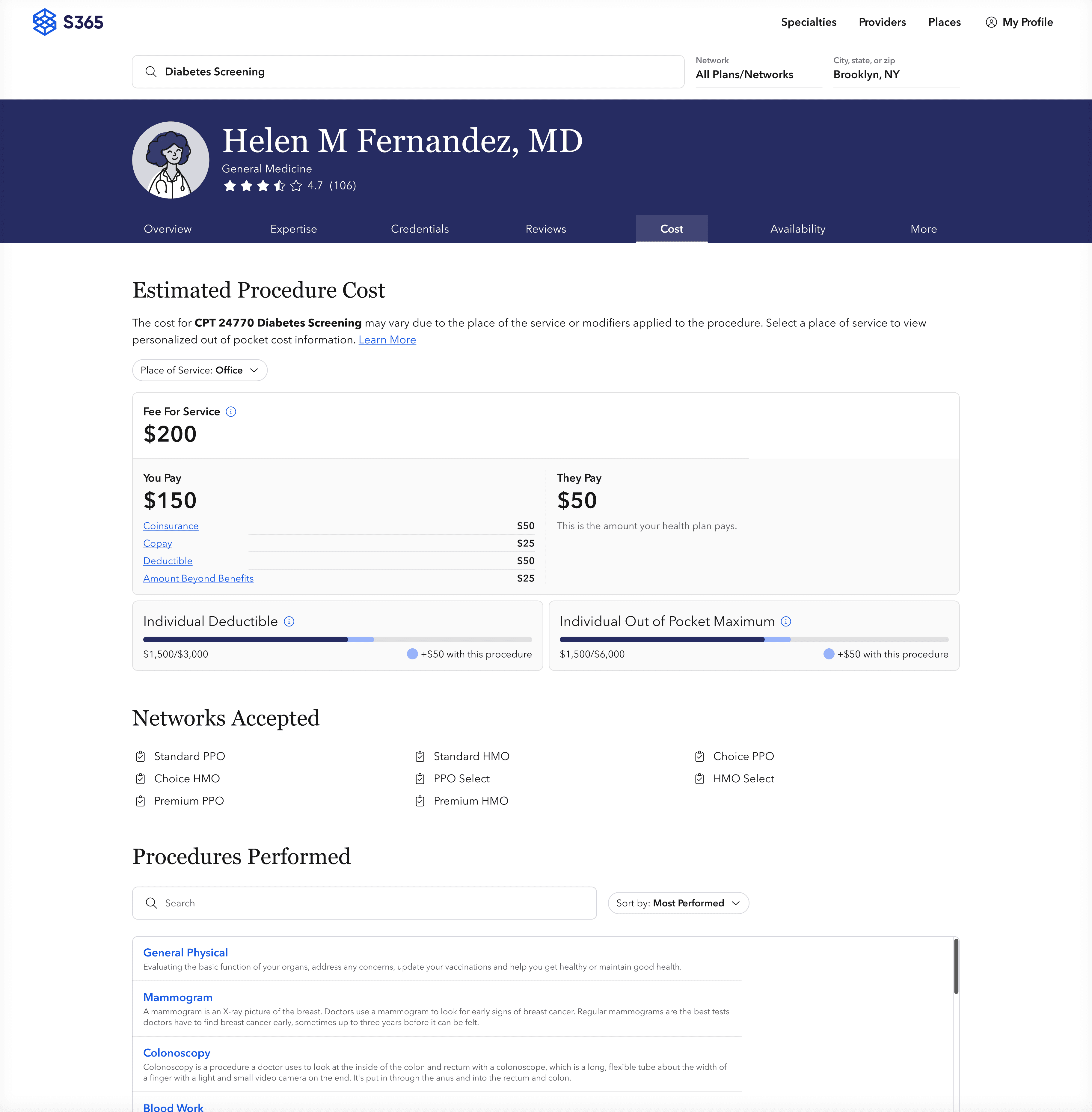
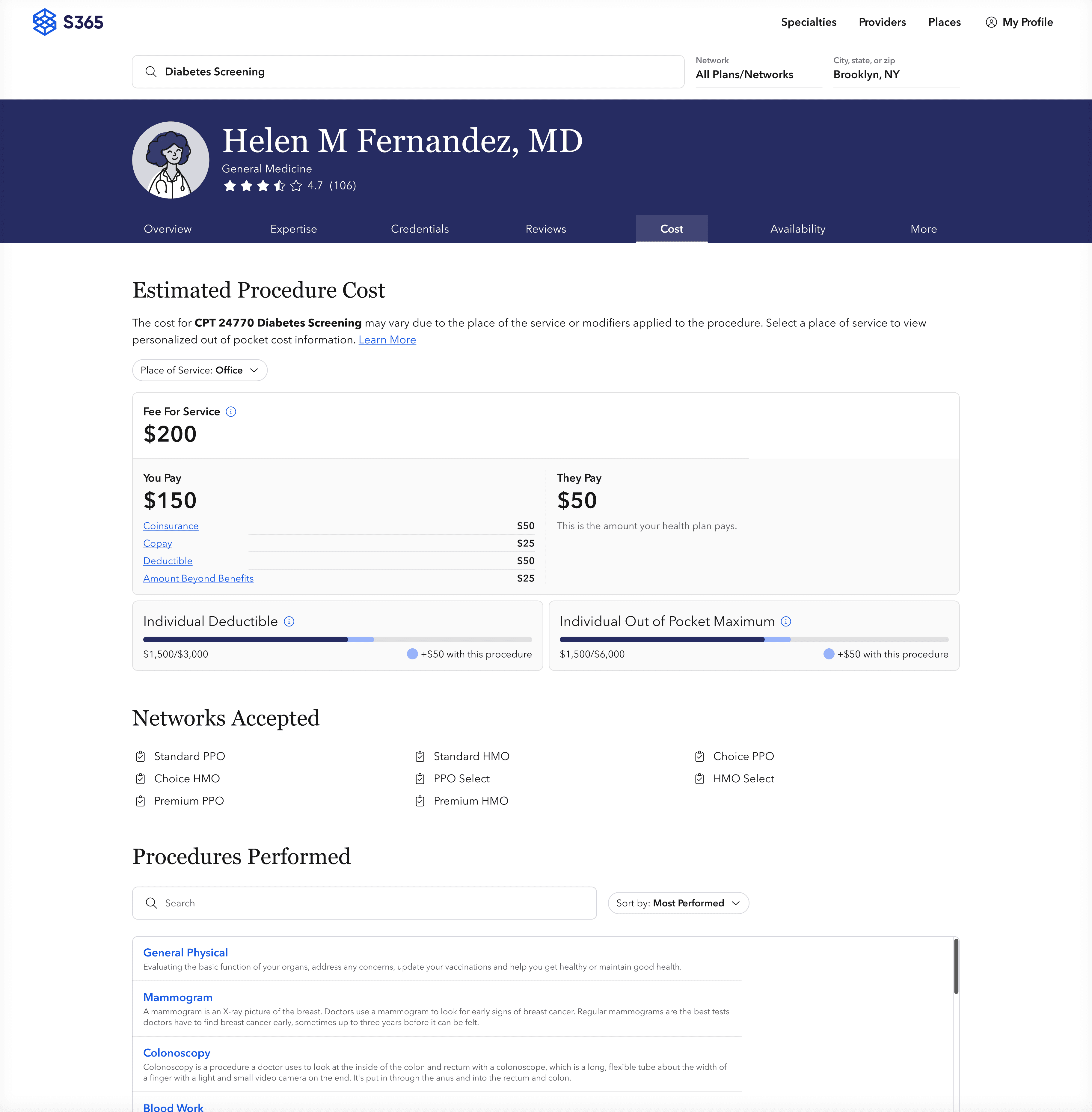
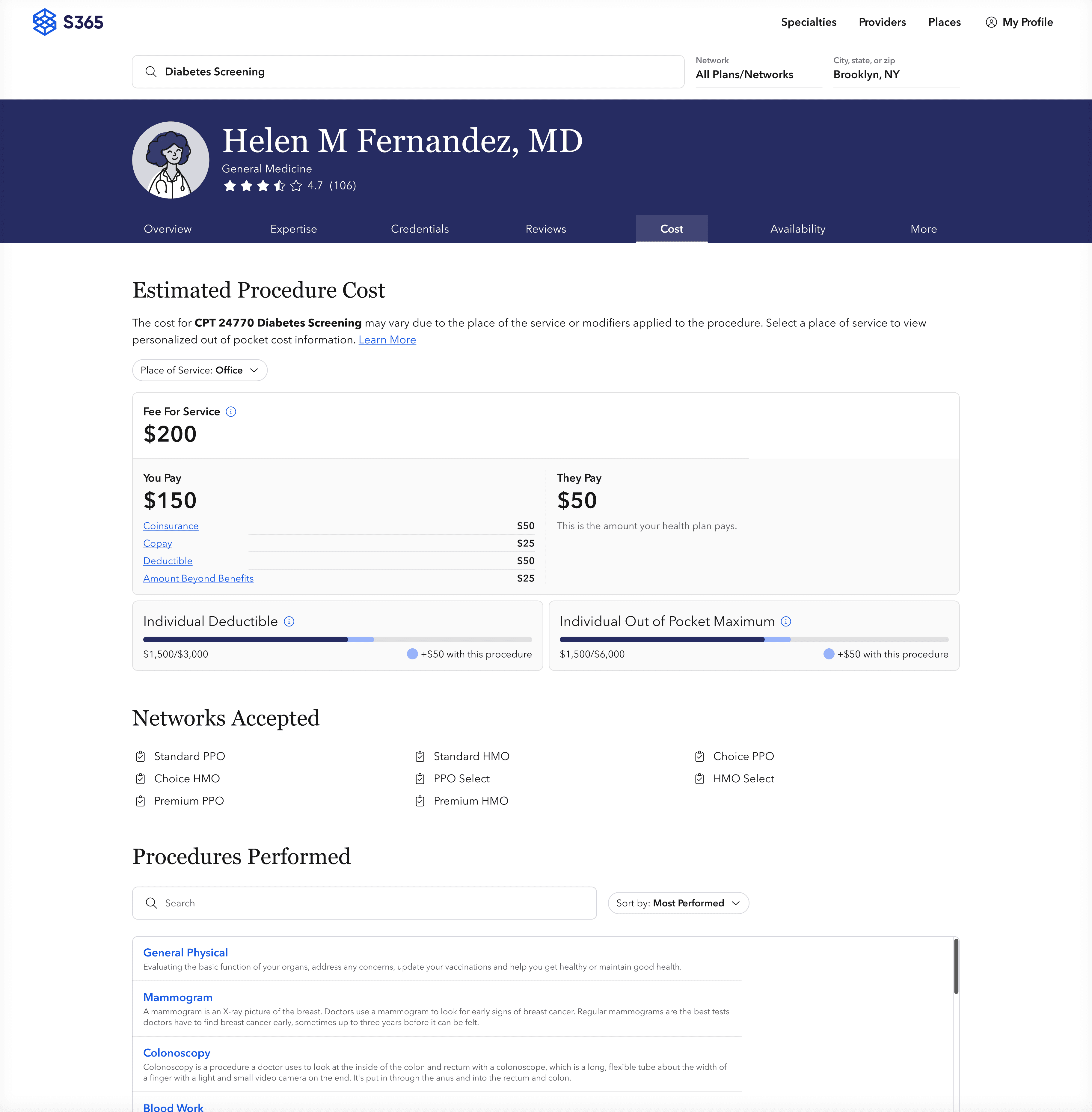
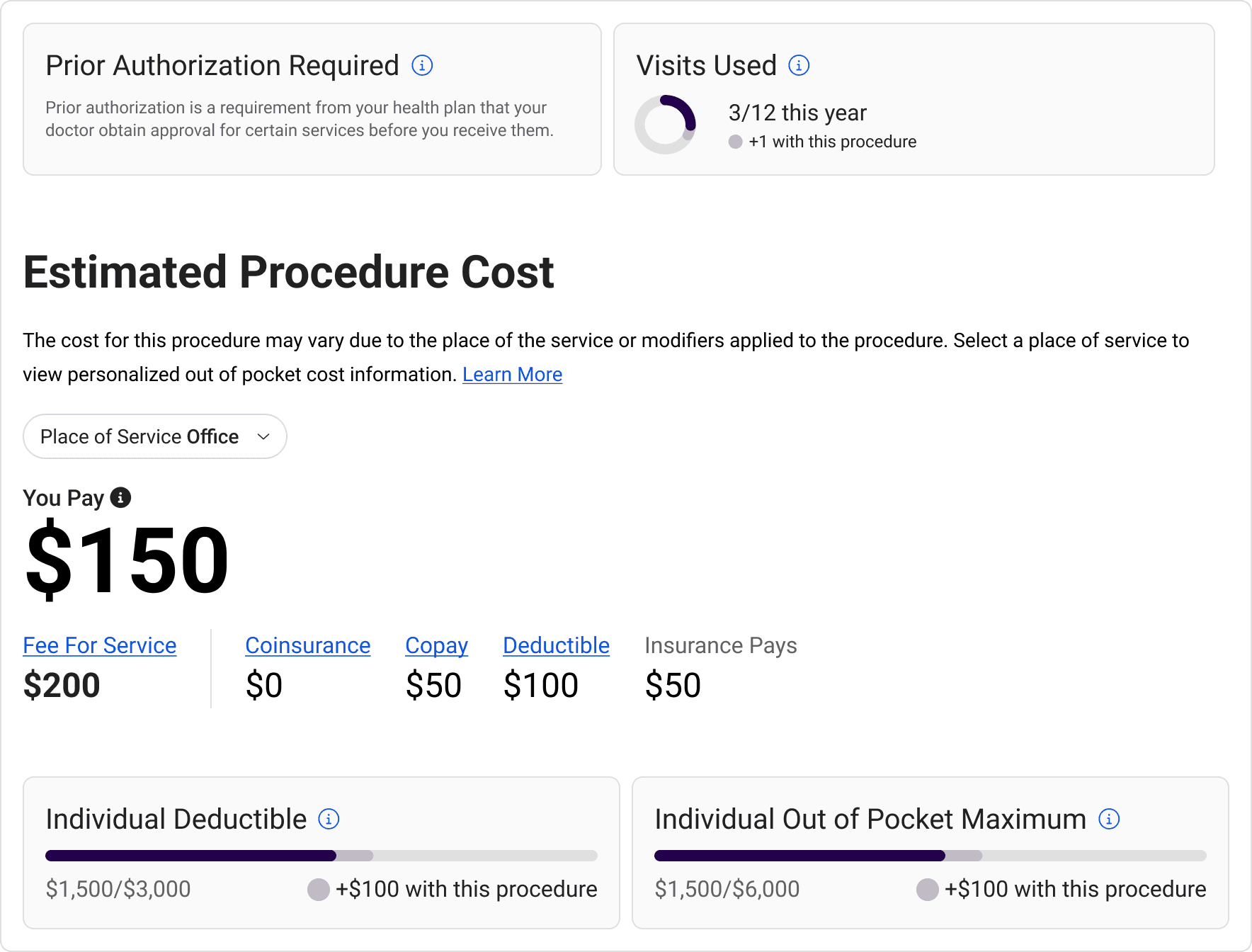
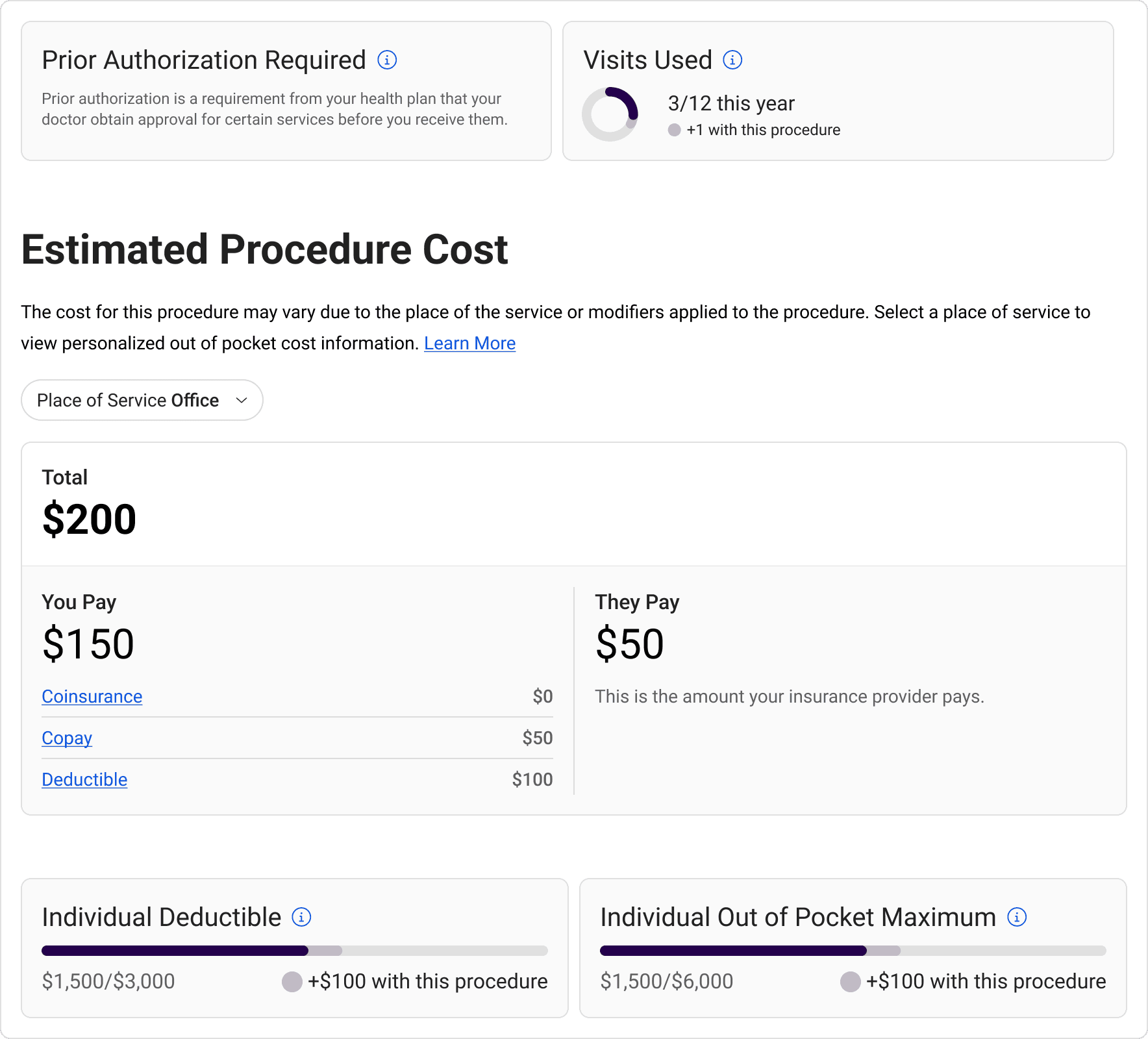
/ Procedure cost card
/ Procedure cost card
/ Procedure cost card
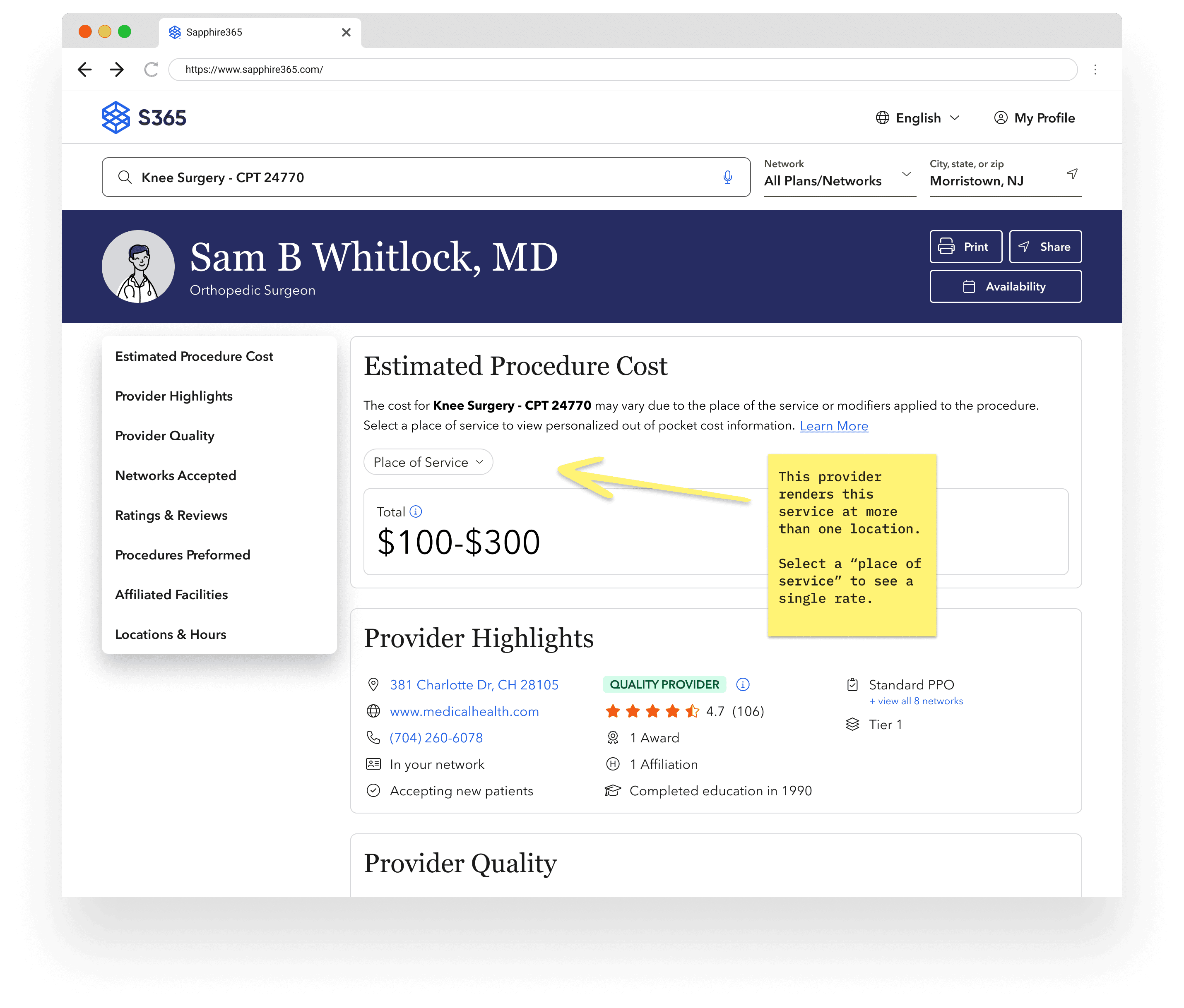
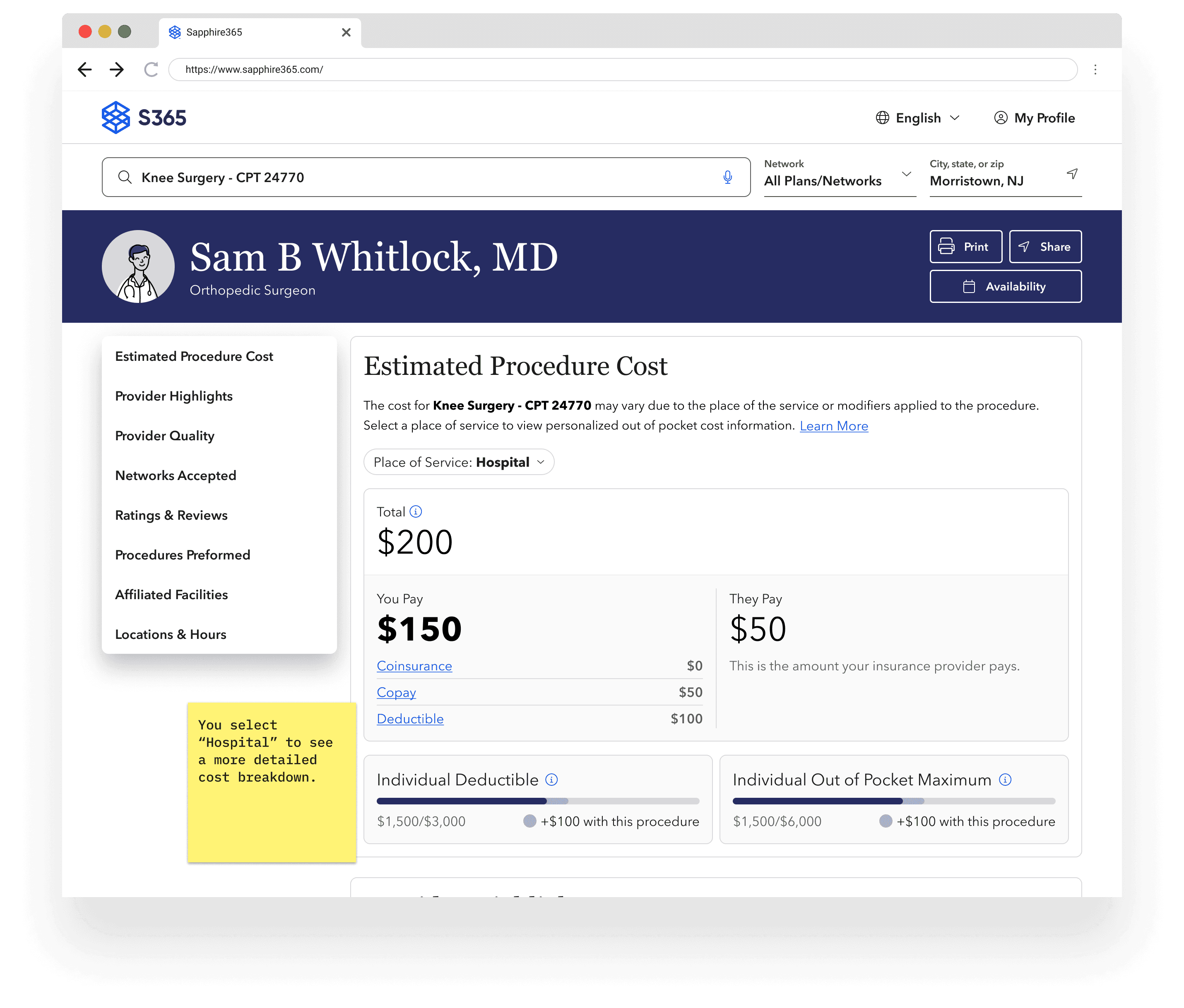
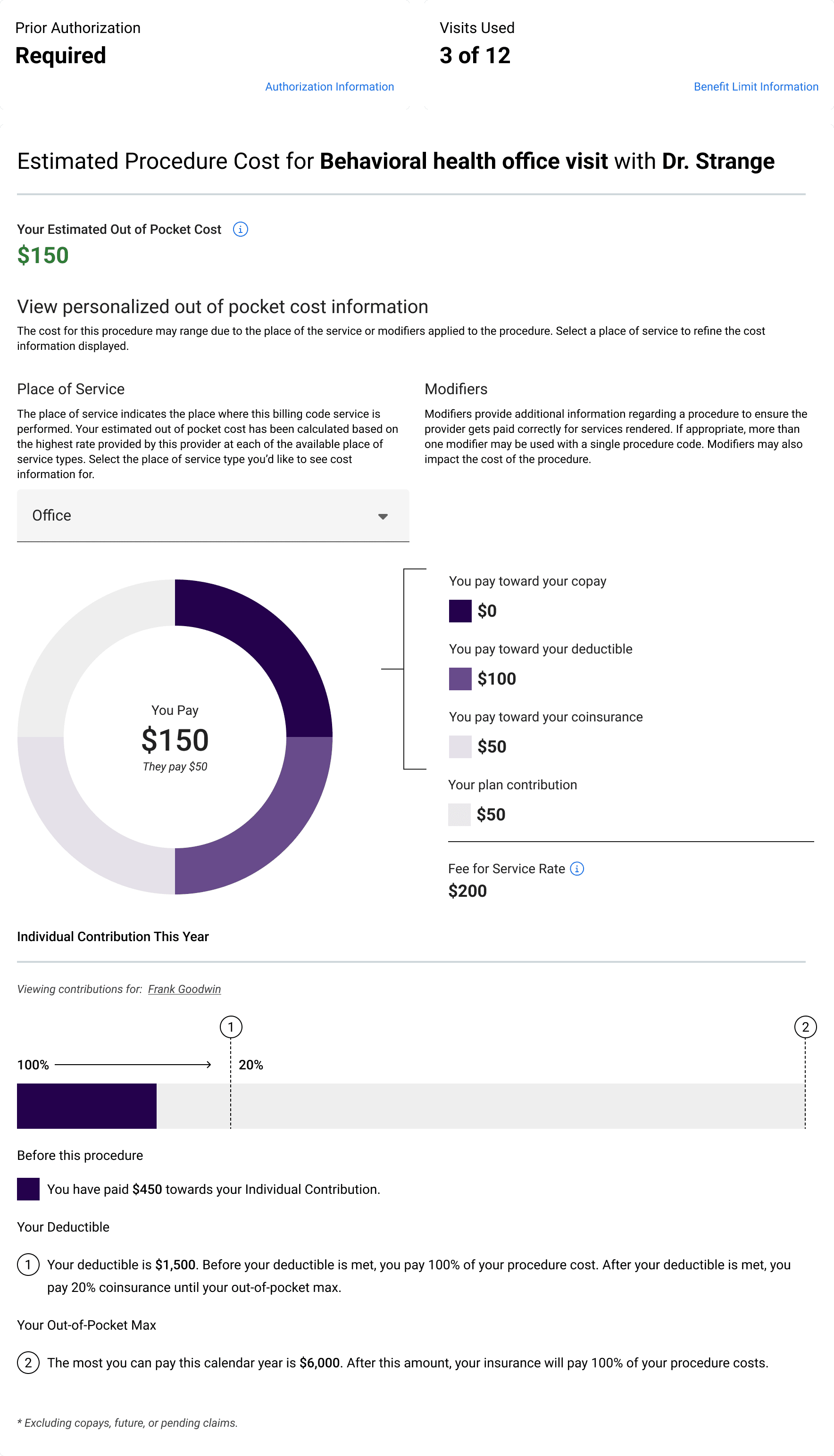
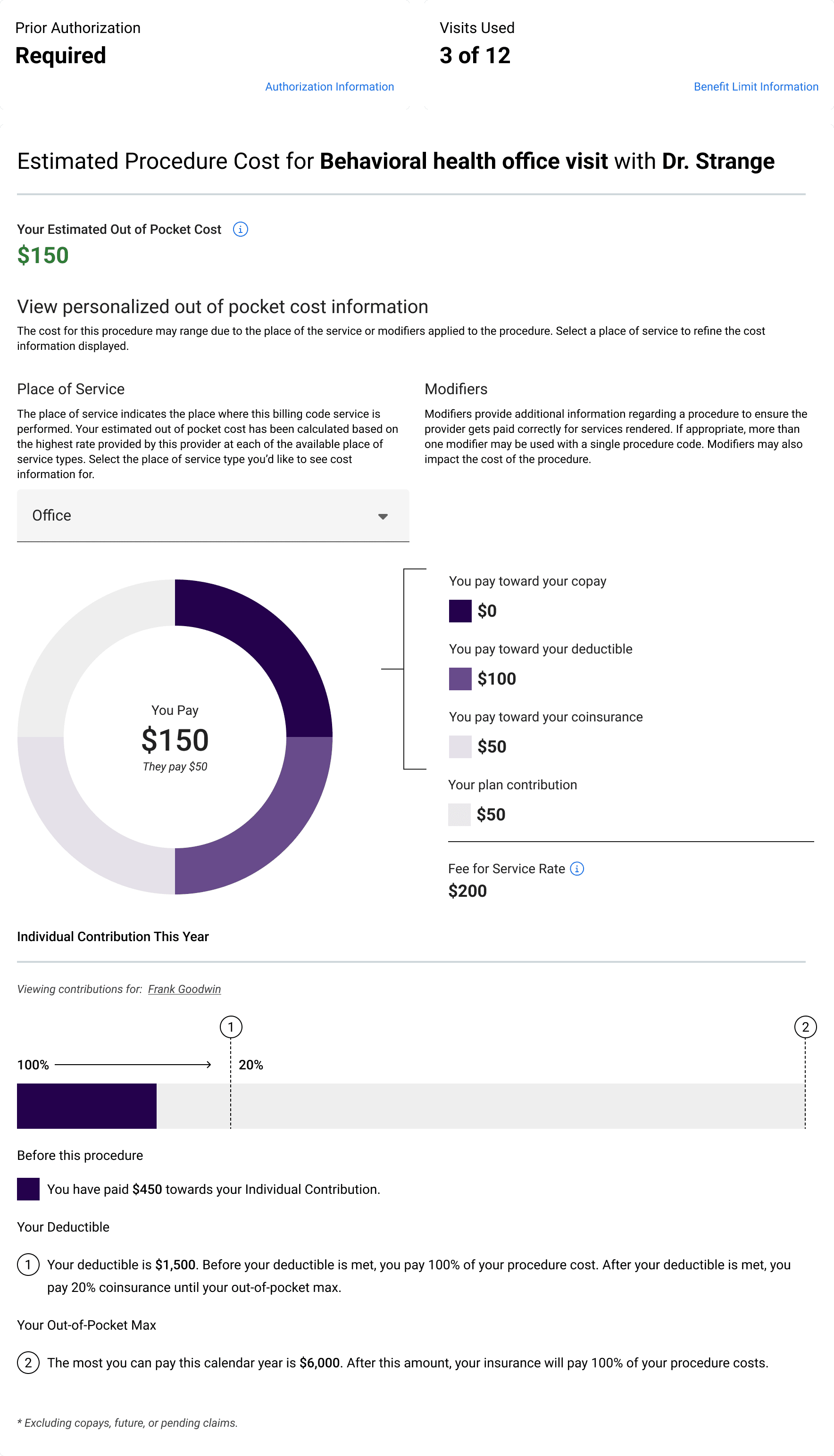
Located on a selected provider’s profile when searching for a procedure, the cost estimate component breaks down applied benefit information to a procedure cost estimate.
Located on a selected provider’s profile when searching for a procedure, the cost estimate component breaks down applied benefit information to a procedure cost estimate.
Located on a selected provider’s profile when searching for a procedure, the cost estimate component breaks down applied benefit information to a procedure cost estimate.
/ Before
/ Before
/ Before
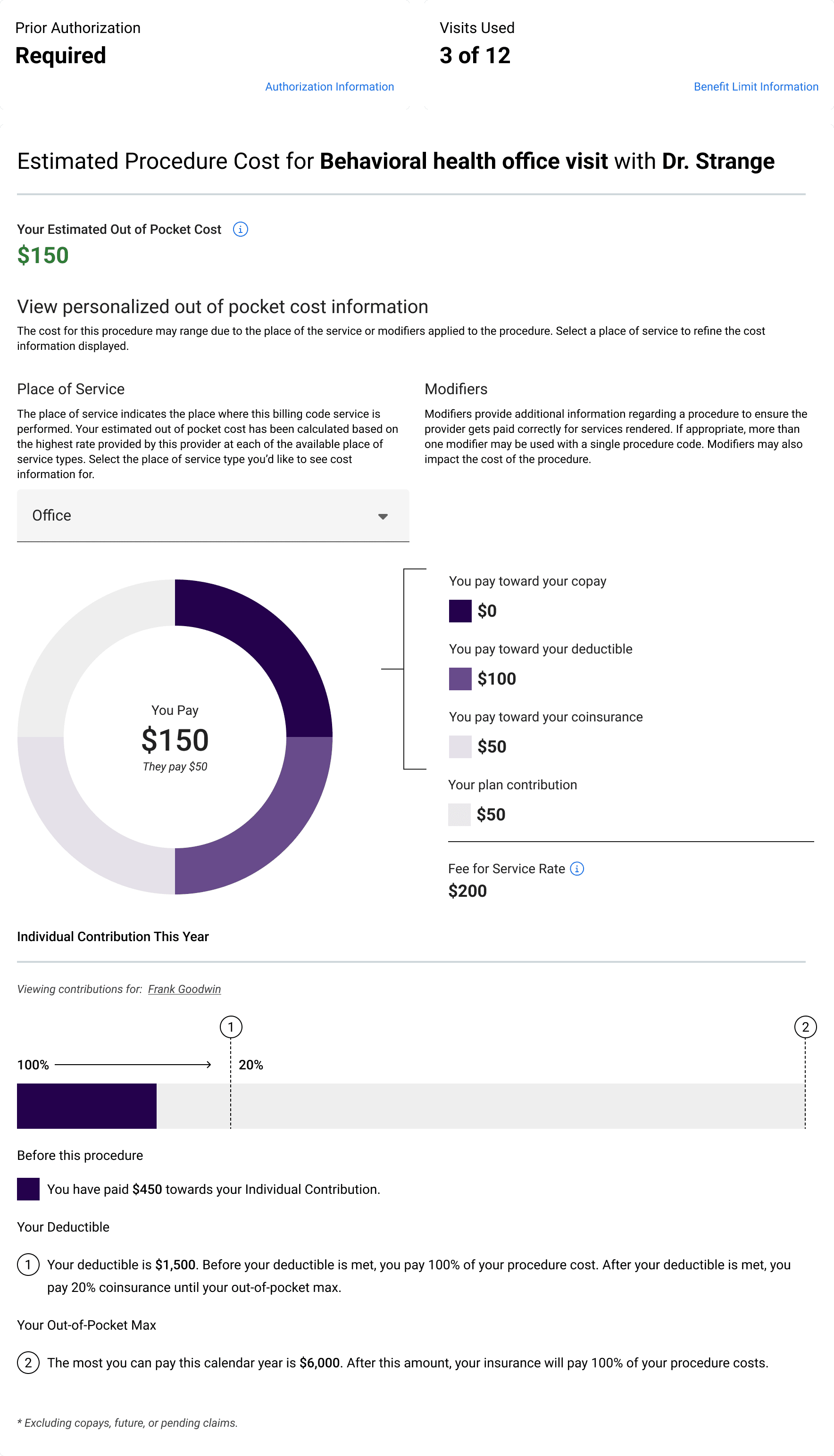
/ Testing
/ Testing
/ Testing
Applying our learnings about healthcare literacy, we conducted a series of usability tests to make procedure cost information more relevant and digestible.
Applying our learnings about healthcare literacy, we conducted a series of usability tests to make procedure cost information more relevant and digestible.
Applying our learnings about healthcare literacy, we conducted a series of usability tests to make procedure cost information more relevant and digestible.
[01]
[02]
[03]
[04]
[05]
[06]
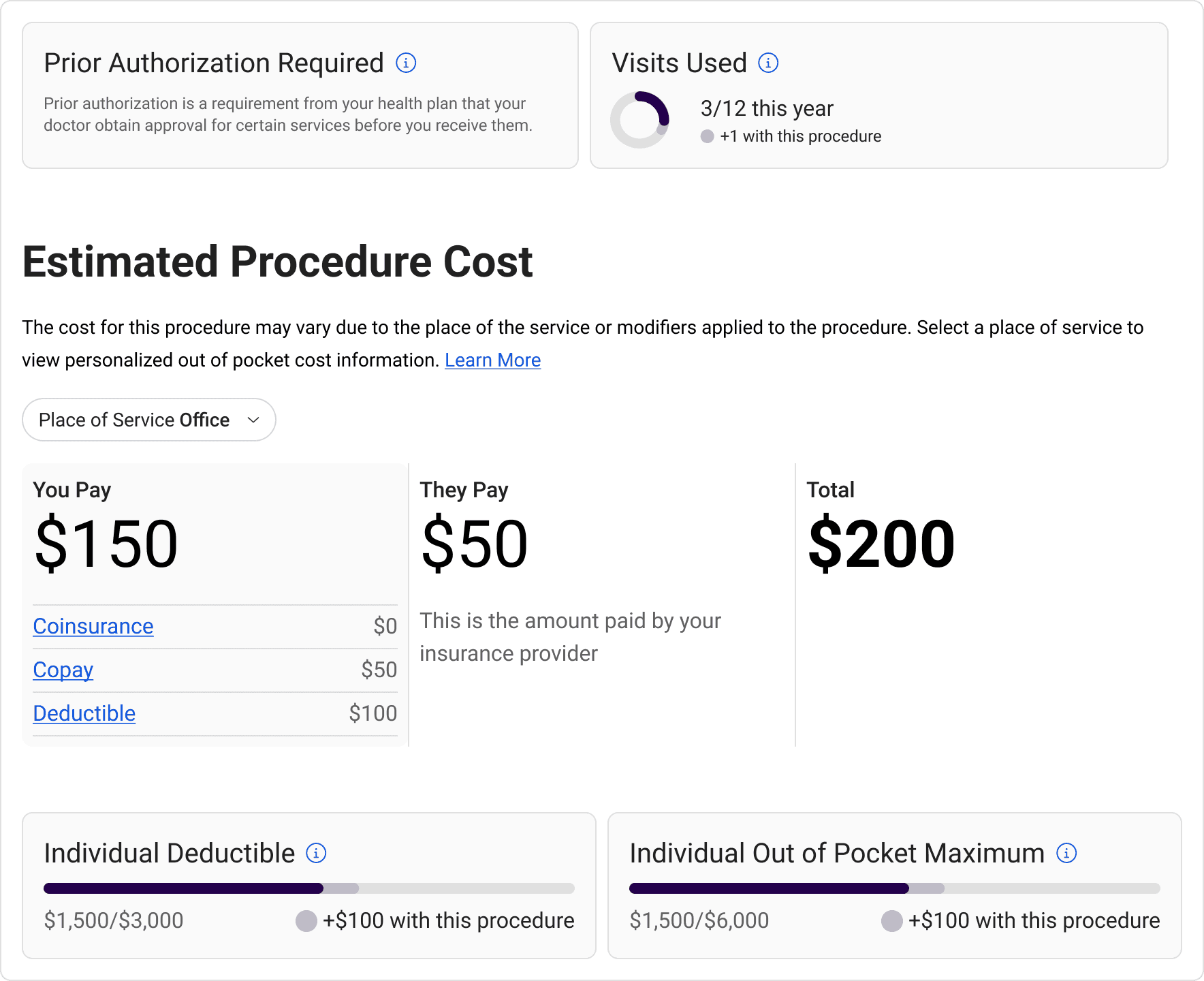
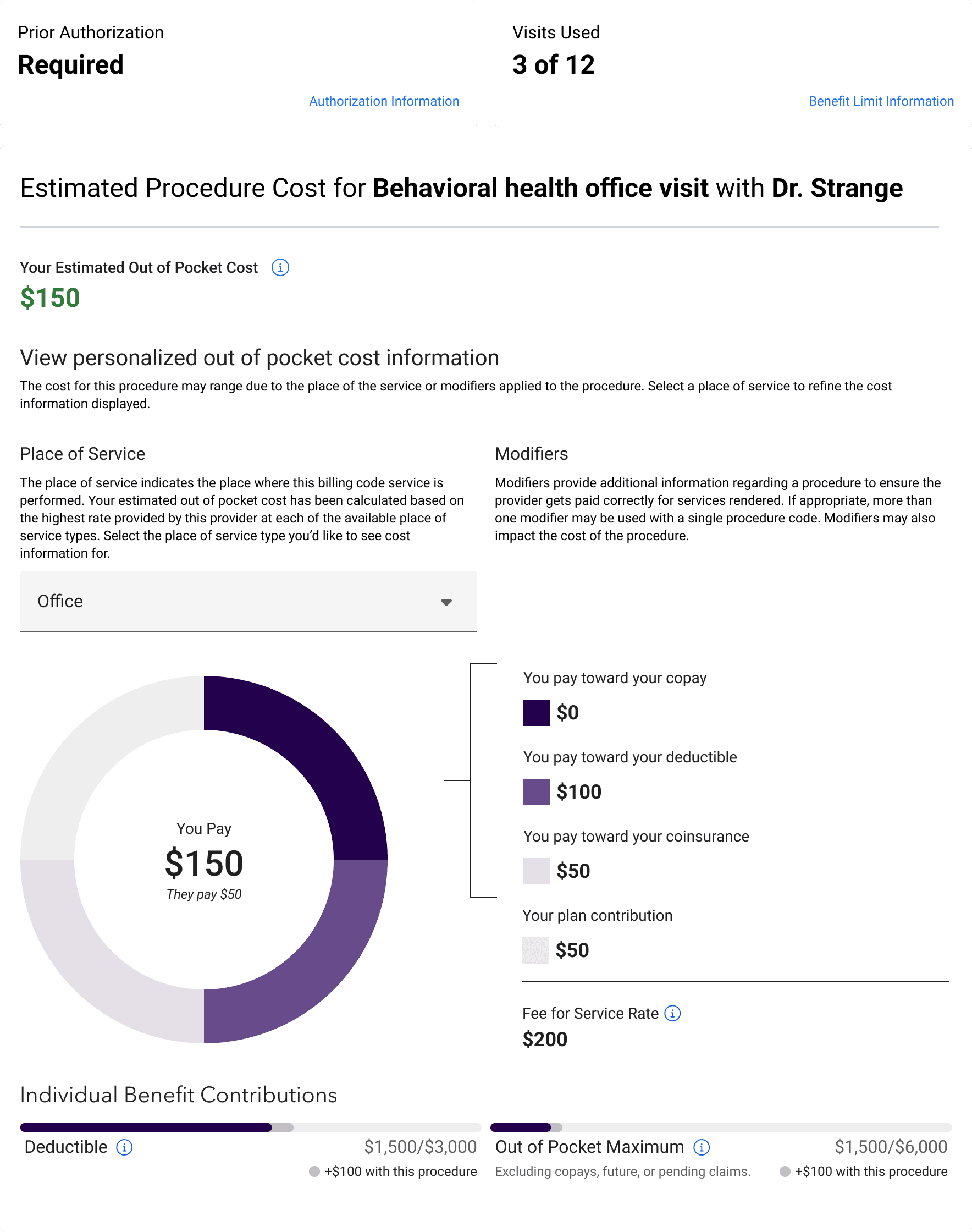
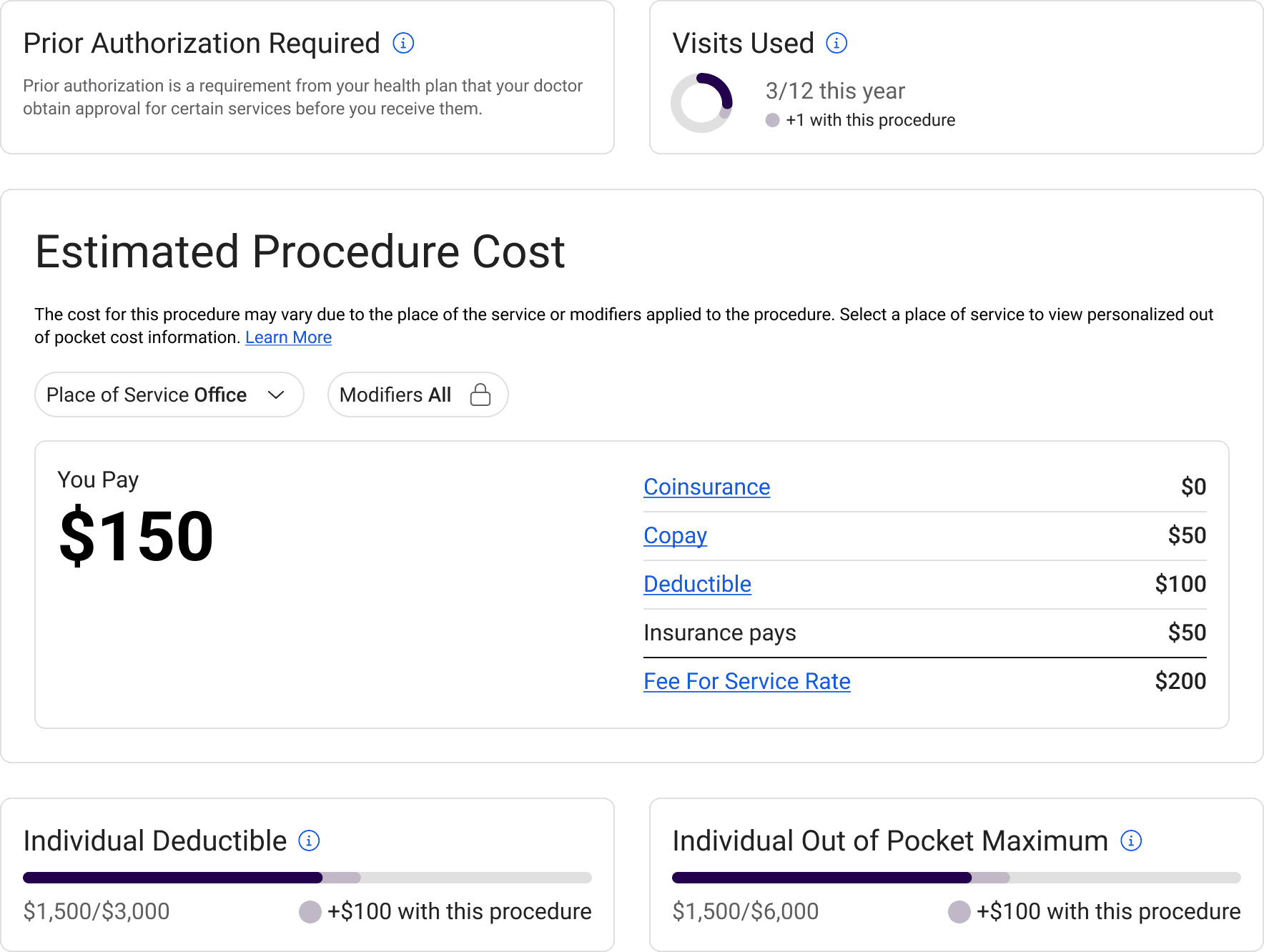
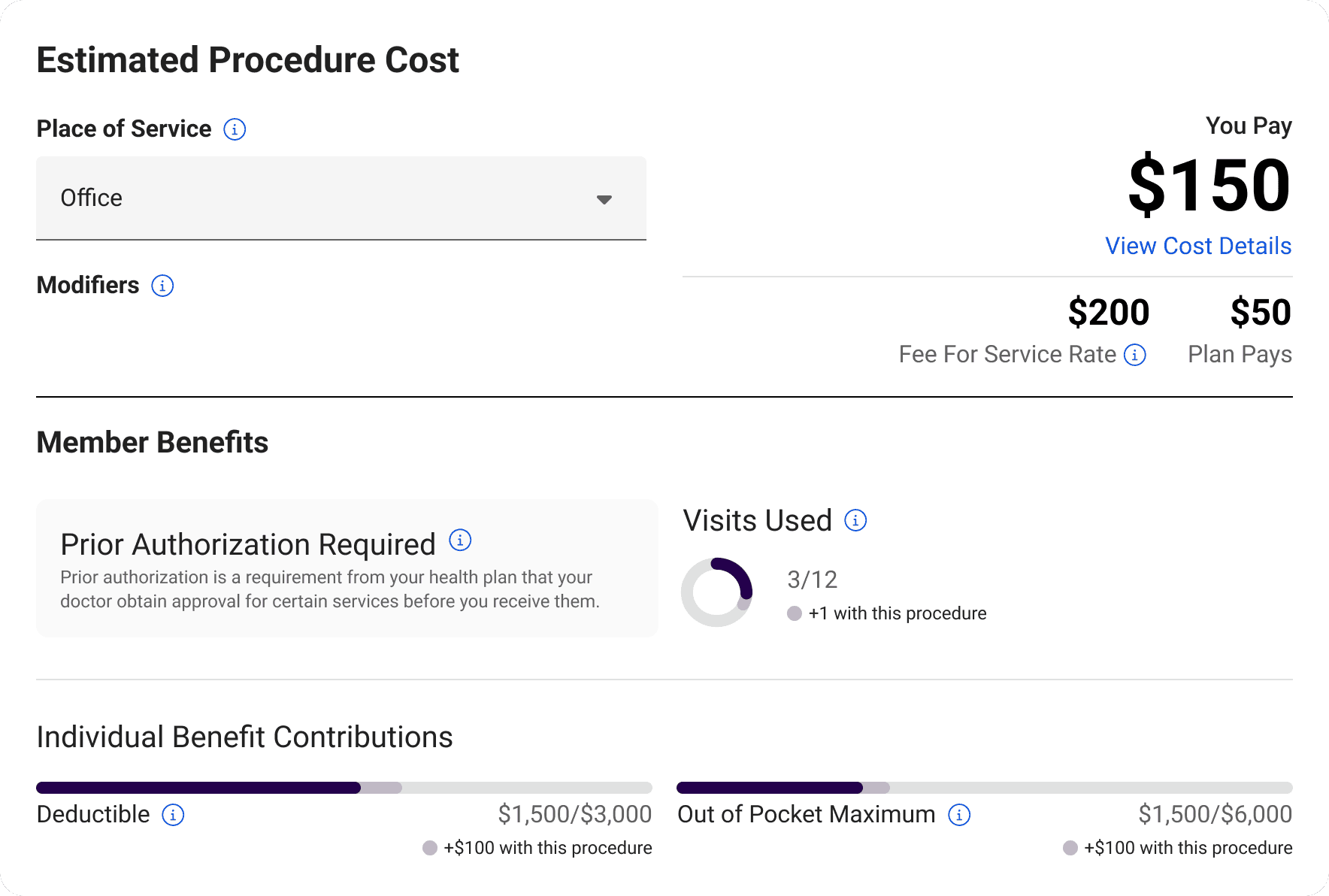
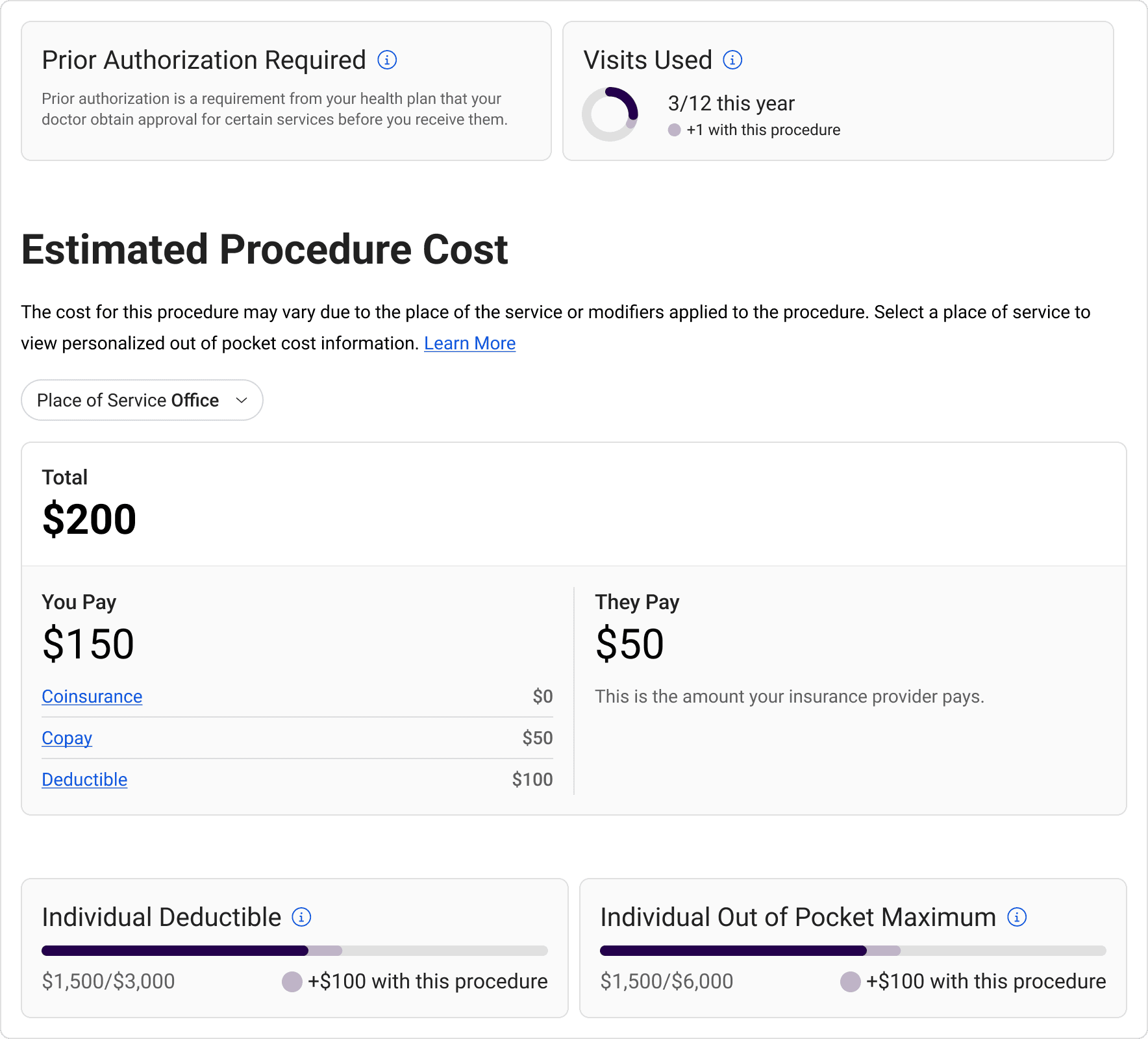
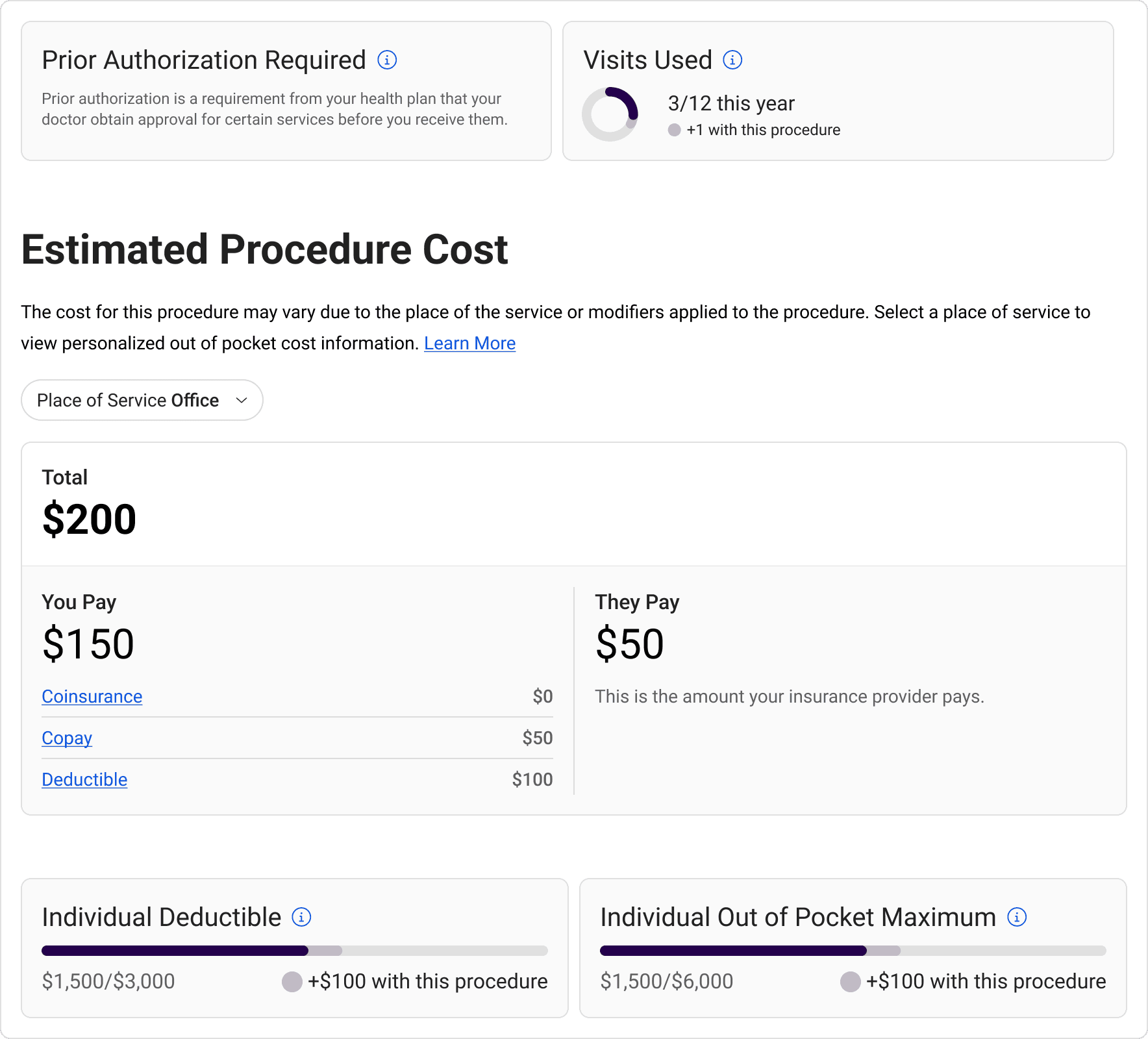
/ Updated cost card
/ Updated cost card
The final design looked to highlight key information while still offering granular breakdowns. We grouped content based on procedure coverage, procedure cost, and benefit accruals to communicate a full procedure cost story.
The final design looked to highlight key information while still offering granular breakdowns. We grouped content based on procedure coverage, procedure cost, and benefit accruals to communicate a full procedure cost story.
/ After
/ Compliance
/ Compliance
/ Compliance
Following the initial 30 UI requirements, all of the developed solutions were documented and signed off by the legal teams of each of our health plan partners.
Following the initial 30 UI requirements, all of the developed solutions were documented and signed off by the legal teams of each of our health plan partners.
Following the initial 30 UI requirements, all of the developed solutions were documented and signed off by the legal teams of each of our health plan partners.
[Part 2]
price competition
among Insurers
price competition
among Insurers
/ Pricing Leverage
/ Pricing Leverage
/ Pricing Leverage
There's a lack of competitive medical pricing leading to excessive patient expenses, which can be attributed to –
There's a lack of competitive medical pricing leading to excessive patient expenses, which can be attributed to –
There's a lack of competitive medical pricing leading to excessive patient expenses, which can be attributed to –
[01]
[01]
[01]
Opaque pricing structures
Opaque pricing structures
Opaque pricing structures
[02]
[02]
[02]
Complex billing processes
Complex billing processes
Complex billing processes
[03]
[03]
[03]
Market consolidation
Market consolidation
Market consolidation
[04]
[04]
[04]
Negotiation power imbalances
Negotiation power imbalances
Negotiation power imbalances
[05]
[05]
[05]
Limited price transparency
Limited price transparency
Limited price transparency
/ Foundation
/ Foundation
/ Foundation
The Network360 tool existed to enable health insurance administrators to see providers in their organizations' networks.
The Network360 tool existed to enable health insurance administrators to see providers in their organizations' networks.
The Network360 tool existed to enable health insurance administrators to see providers in their organizations' networks.
/ Before
/ Before
/ Before
Insures want more money,
So they increase prices.
Insures want more money,
So they increase prices.
Insures want more money,
So they increase prices.
Patients are financially uninformed,
So they’re forced to pay anything.
Patients are financially uninformed,
So they’re forced to pay anything.
Patients are financially uninformed,
So they’re forced to pay anything.
/ After
/ After
/ After
Users can choose affordable care,
So they steer pricing by demand.
Users can choose affordable care,
So they steer pricing by demand.
Users can choose affordable care,
So they steer pricing by demand.
Insures need to retain members,
So they’re forced to negotiate competitively.
Insures need to retain members,
So they’re forced to negotiate competitively.
Insures need to retain members,
So they’re forced to negotiate competitively.
/ Data Navigation
/ Data Navigation
/ Data Navigation
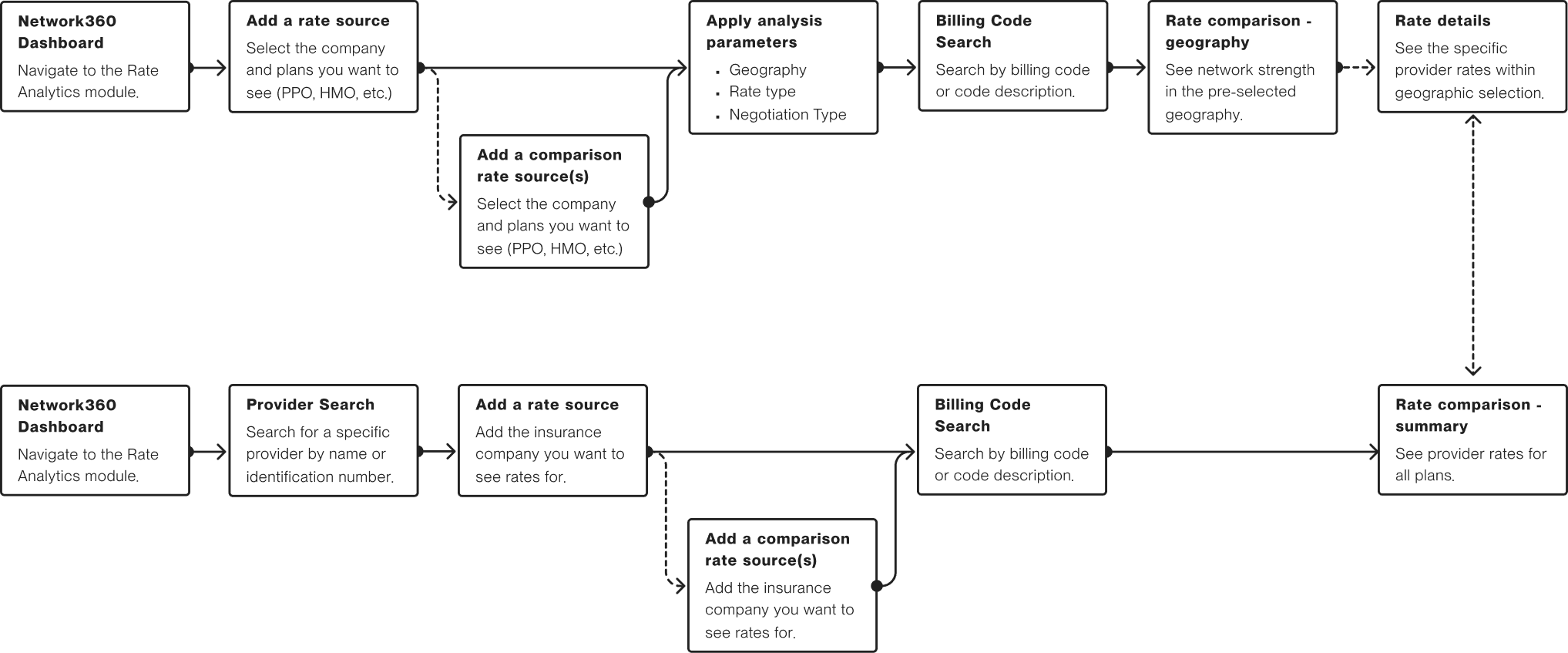
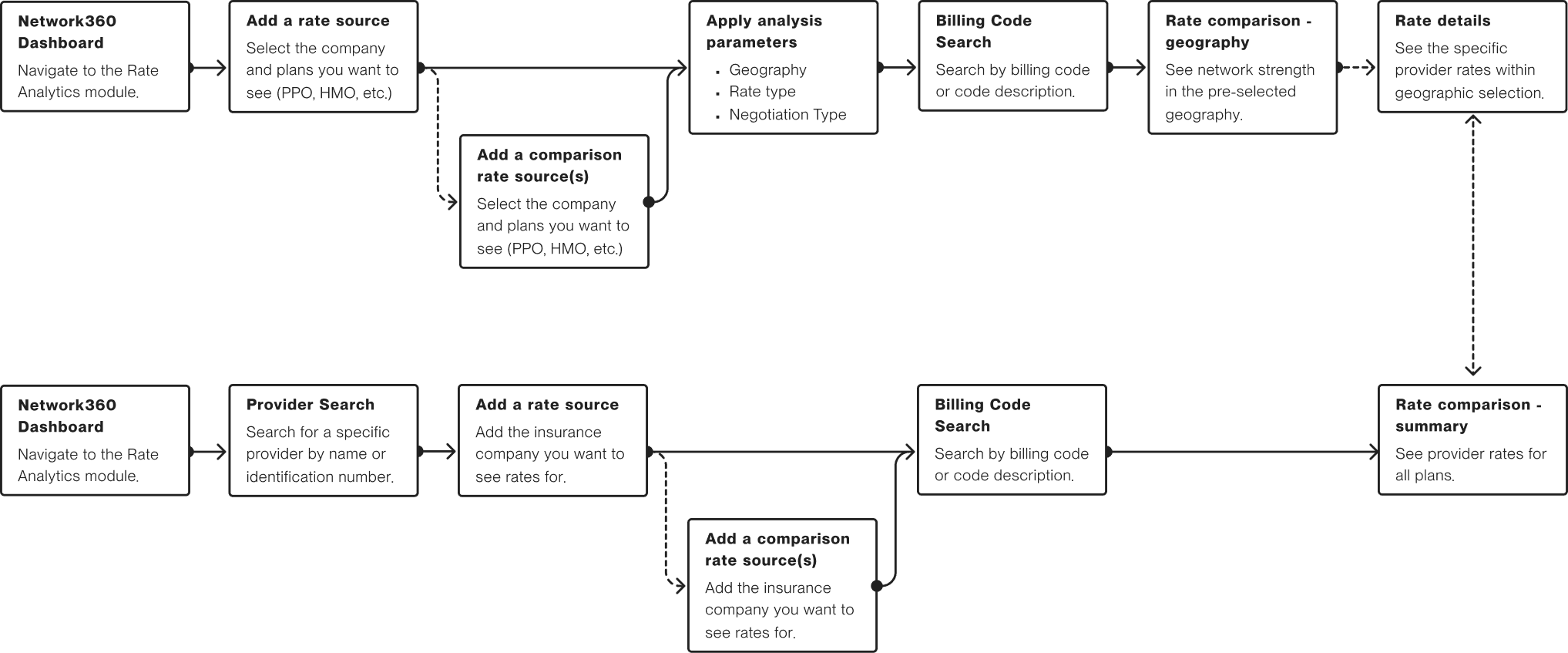
When looking for rate information, a network administrator may be looking for specific details or network patterns. Our user testing informed top-down (network first) and bottom-up (provider first) methods of navigating rate information.
When looking for rate information, a network administrator may be looking for specific details or network patterns. Our user testing informed top-down (network first) and bottom-up (provider first) methods of navigating rate information.
When looking for rate information, a network administrator may be looking for specific details or network patterns. Our user testing informed top-down (network first) and bottom-up (provider first) methods of navigating rate information.
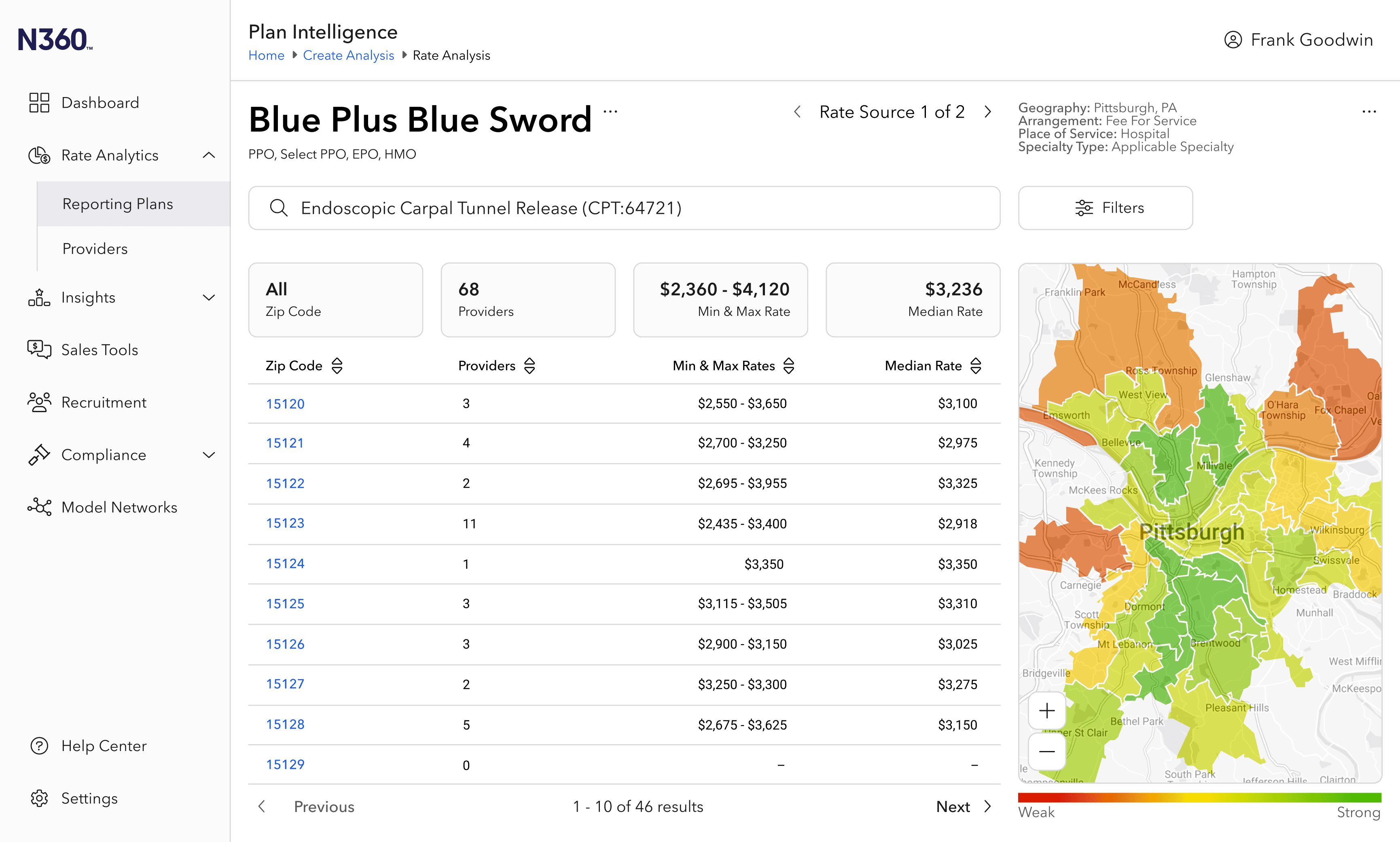
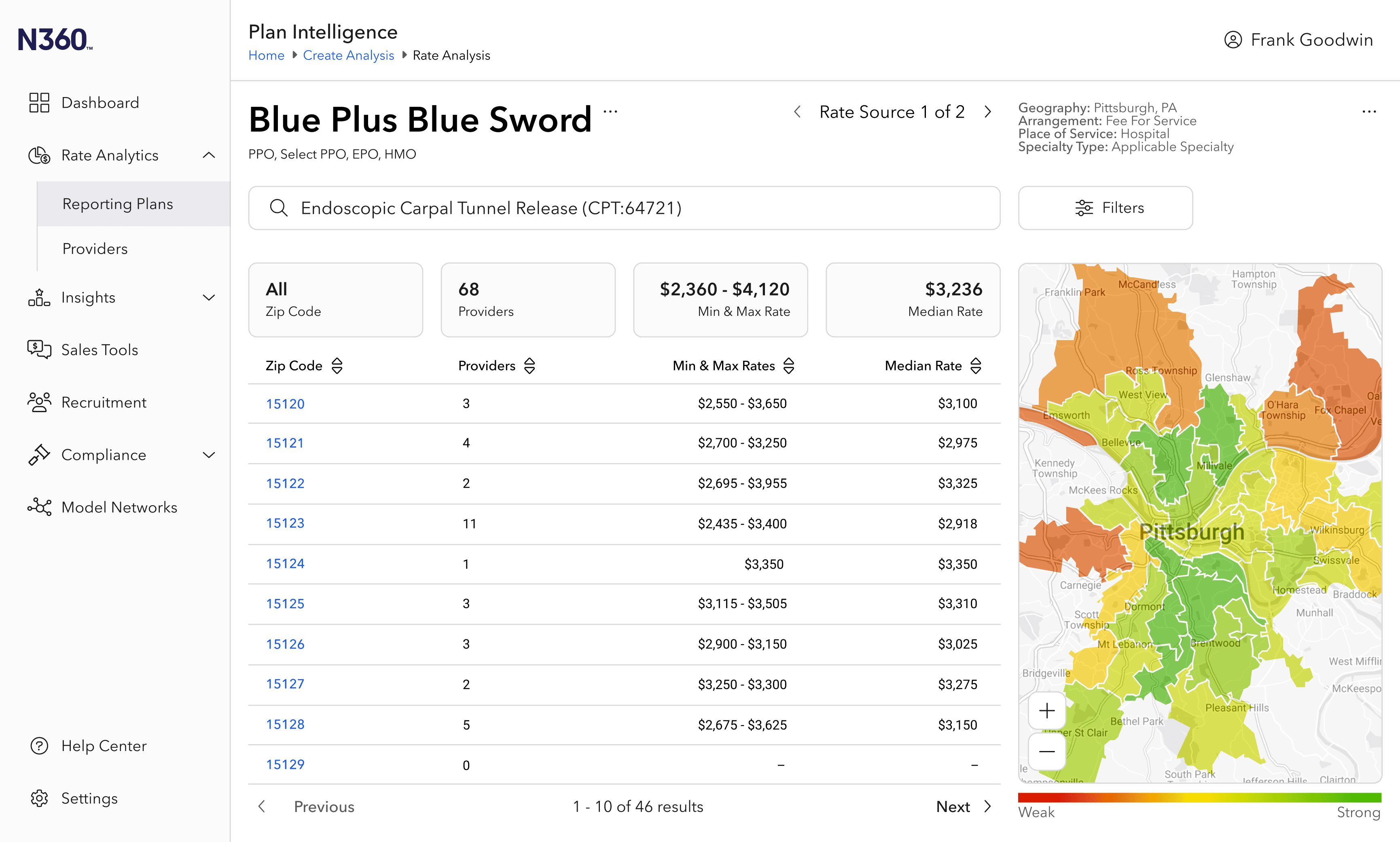
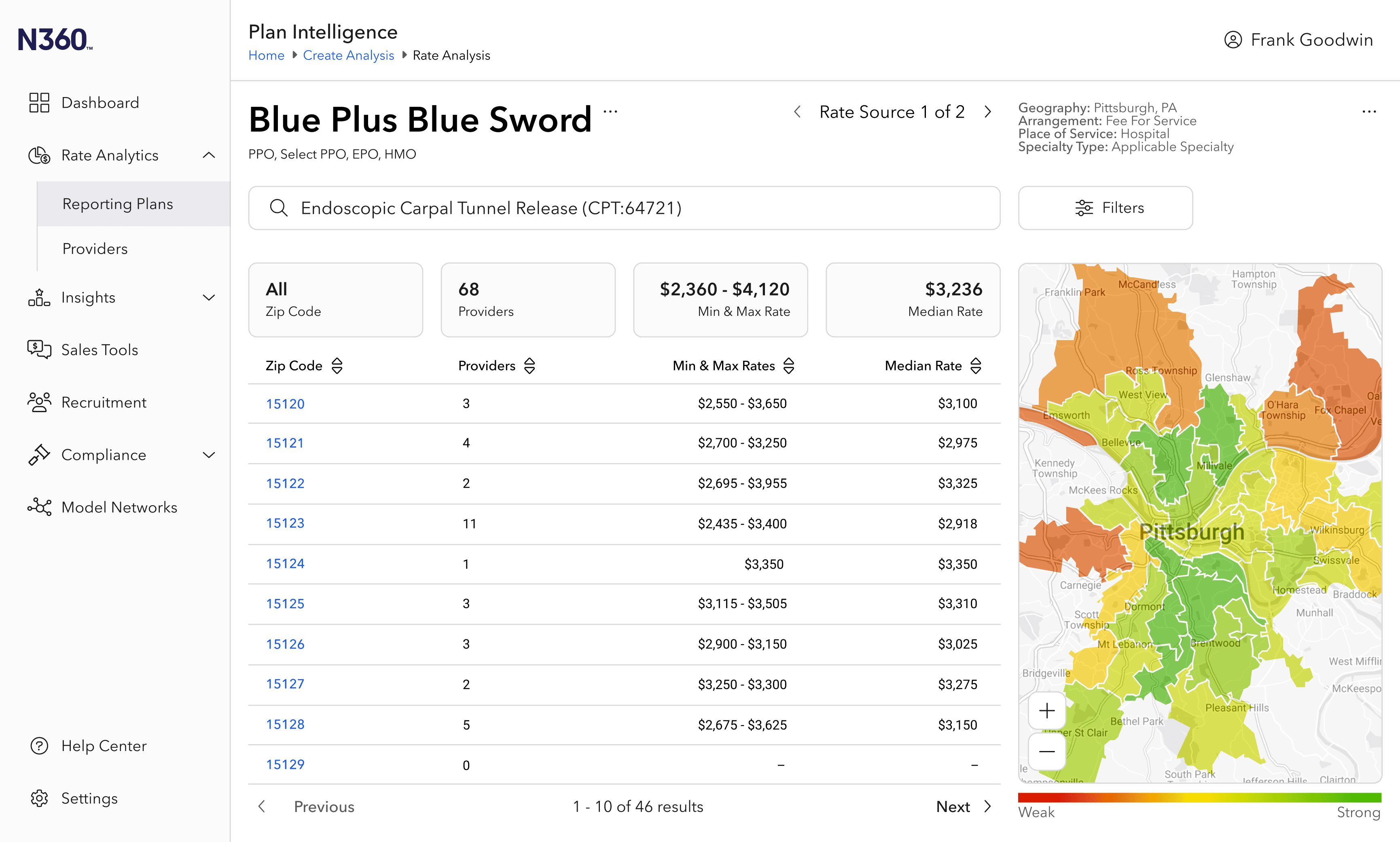
/ Rate Analytics
/ Rate Analytics
/ Rate Analytics
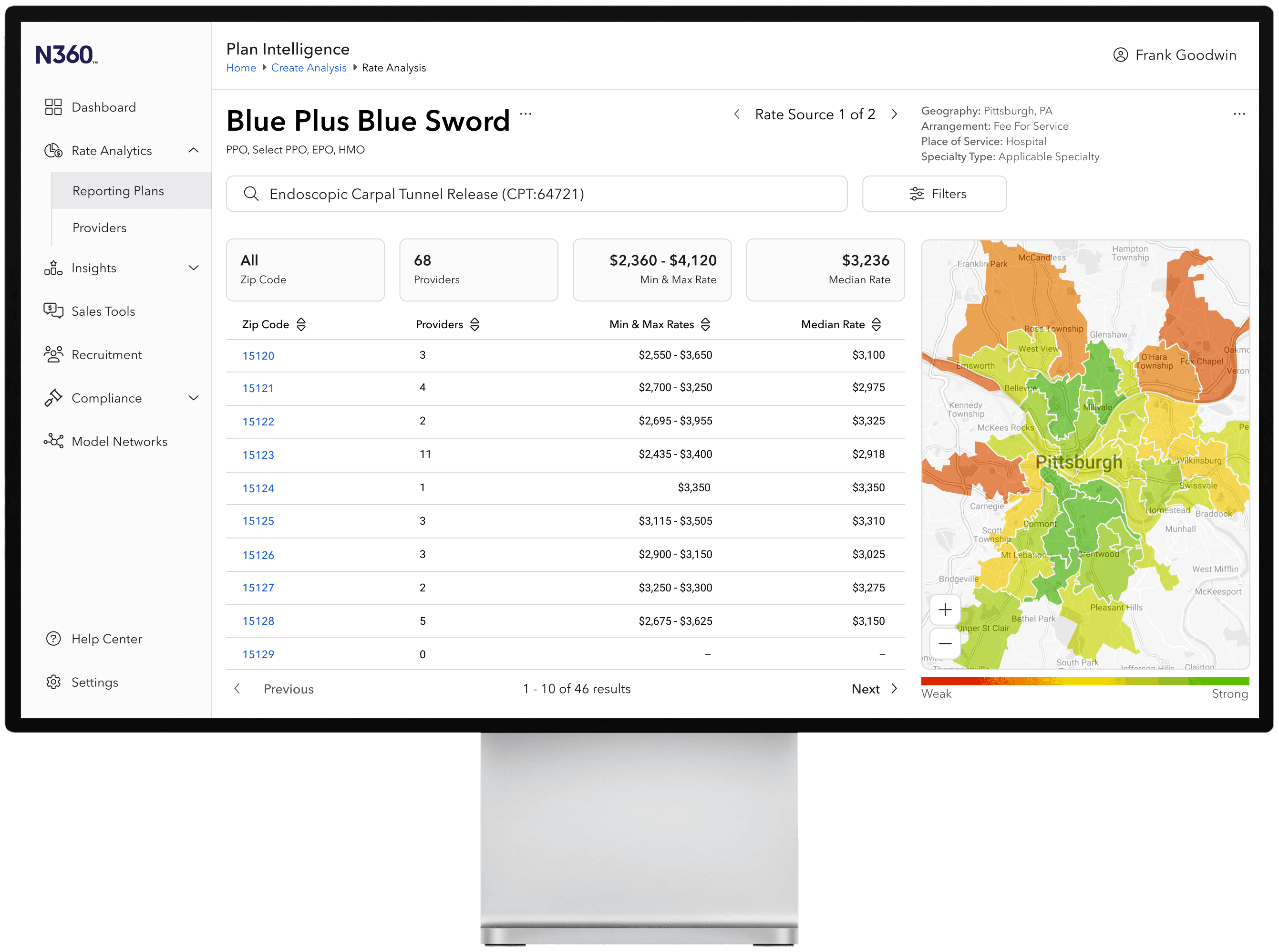
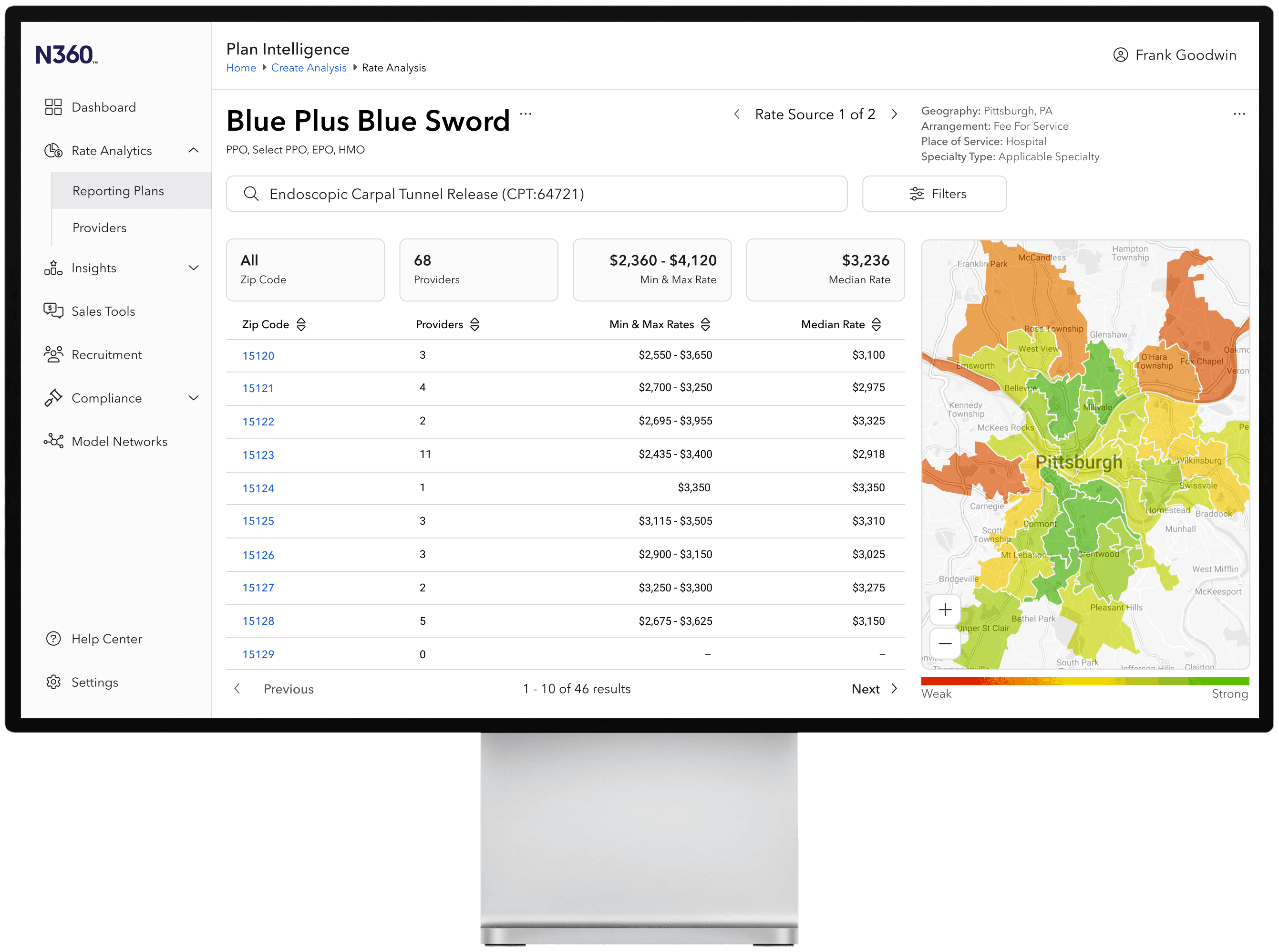
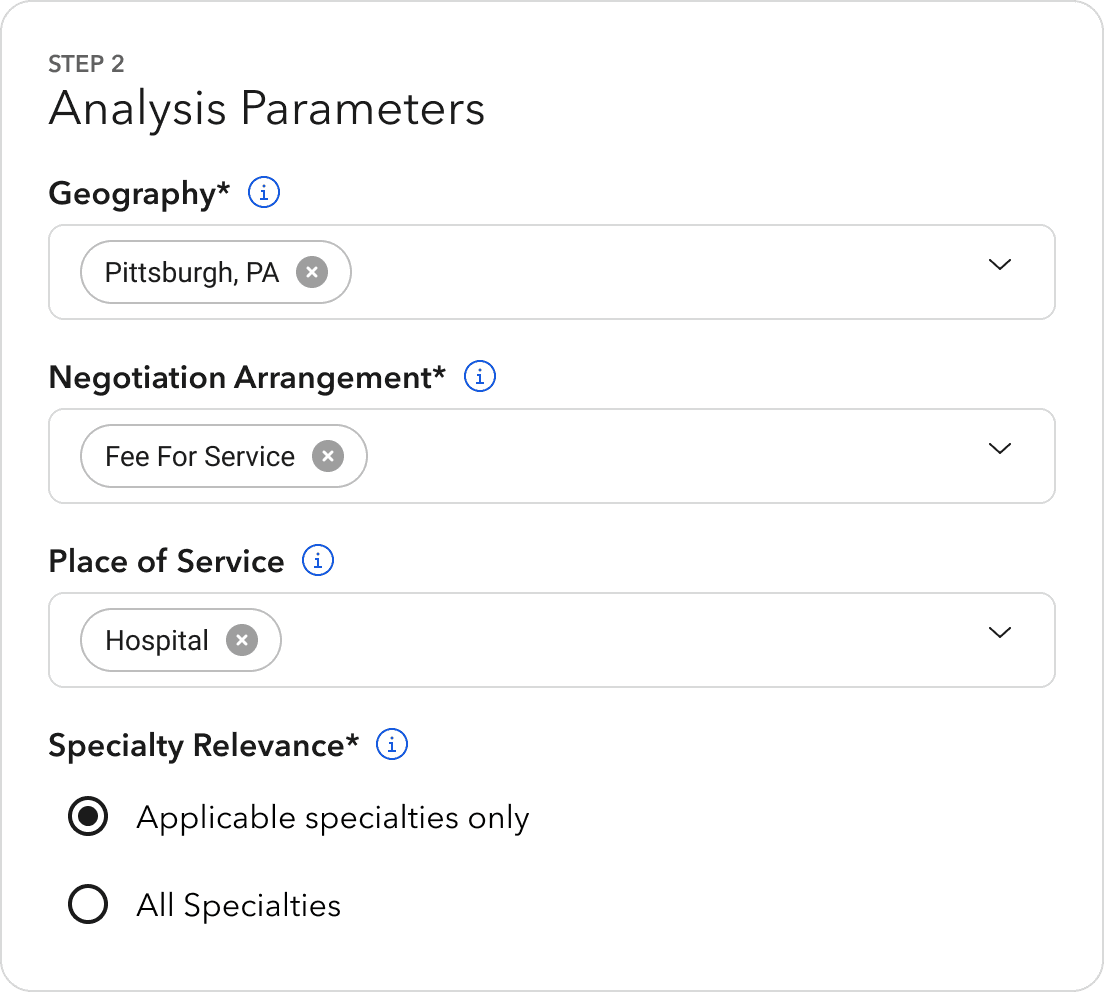
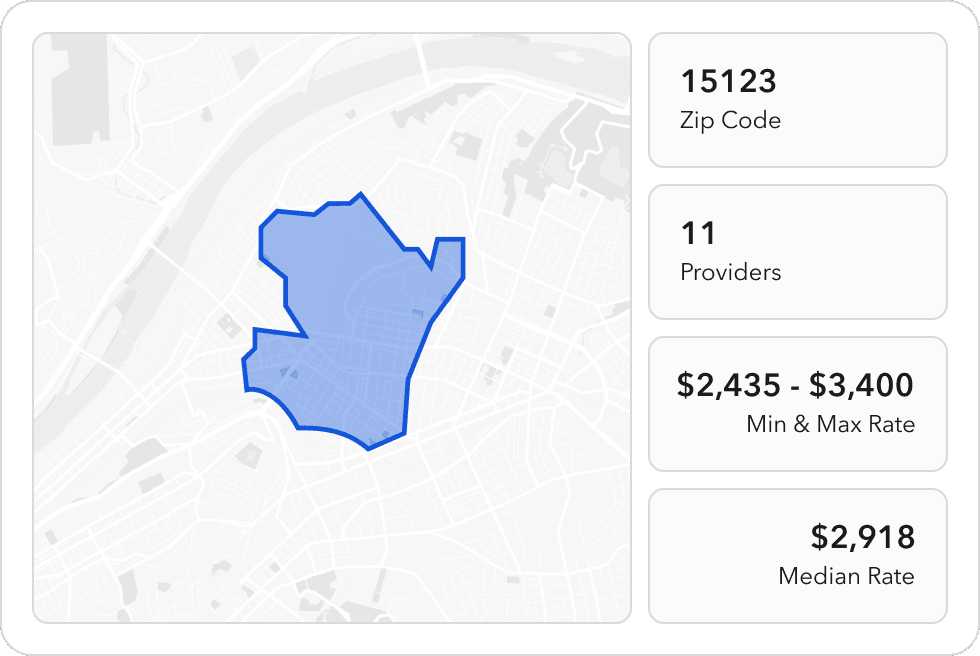
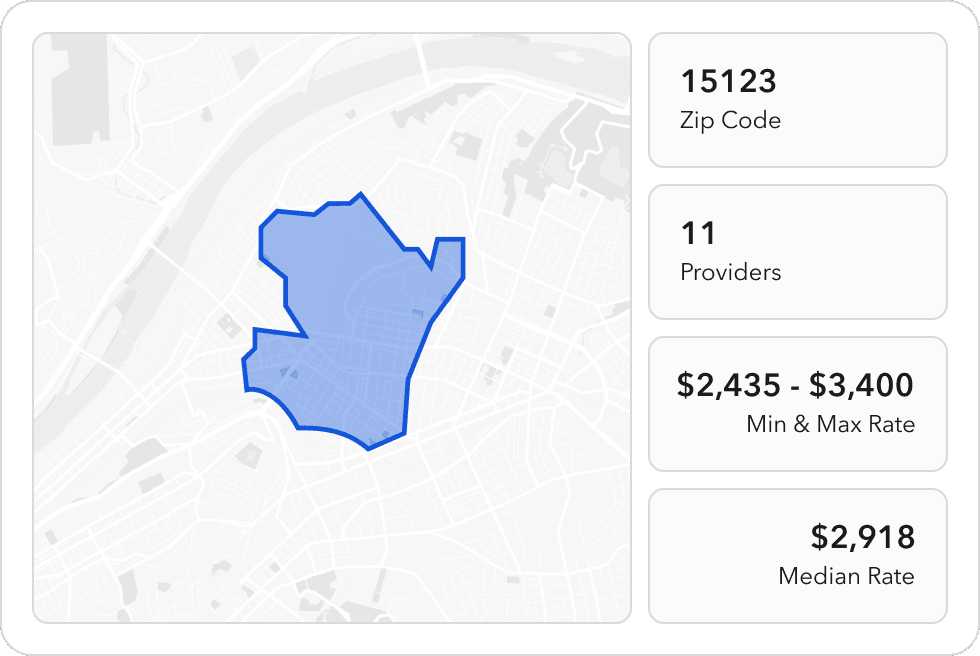
Named "Rate Analytics", the new module delivers a data analysis tool with data visualizations and enhanced provider network segmentation.
Named "Rate Analytics", the new module delivers a data analysis tool with data visualizations and enhanced provider network segmentation.
Named "Rate Analytics", the new module delivers a data analysis tool with data visualizations and enhanced provider network segmentation.
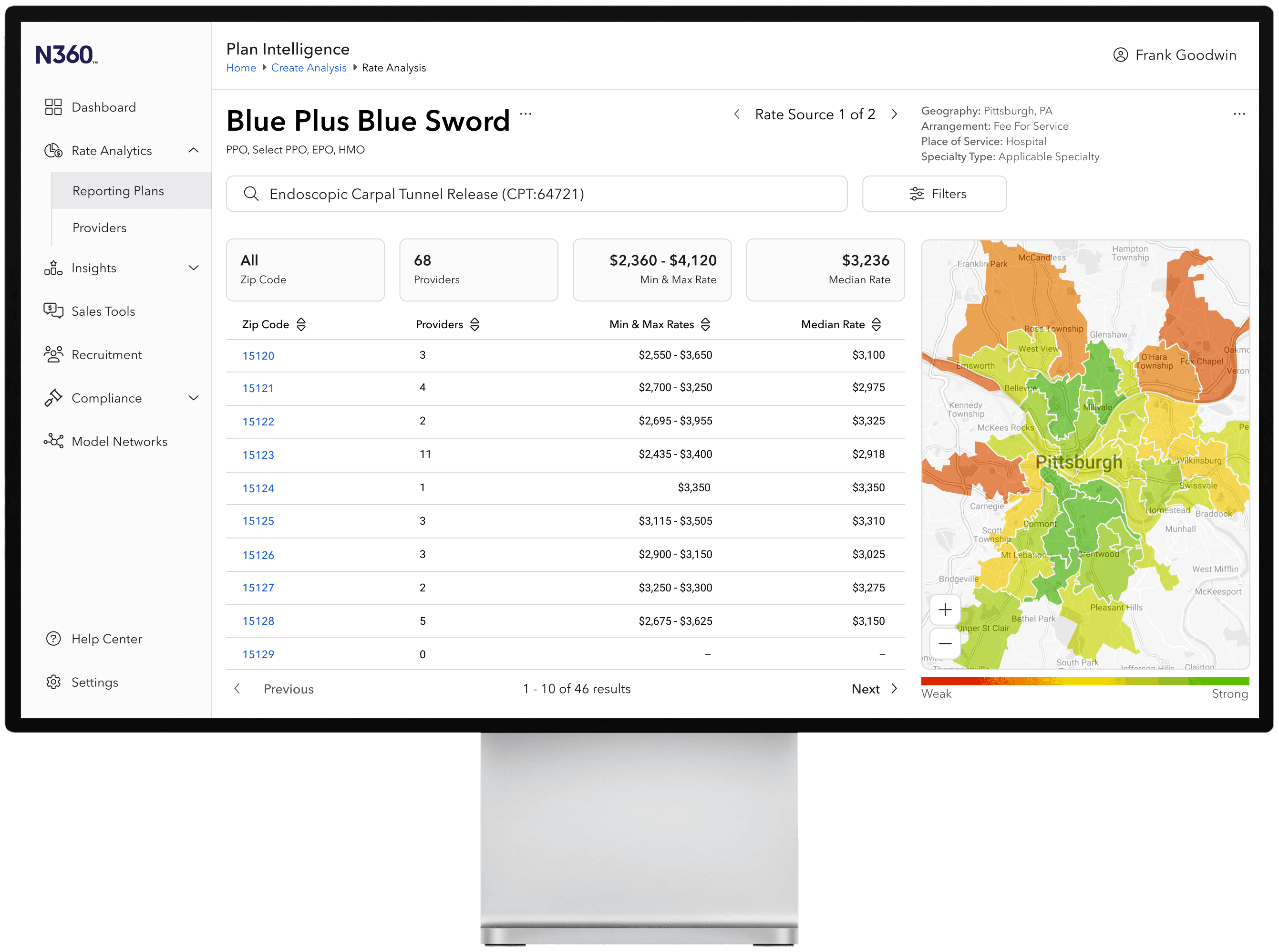
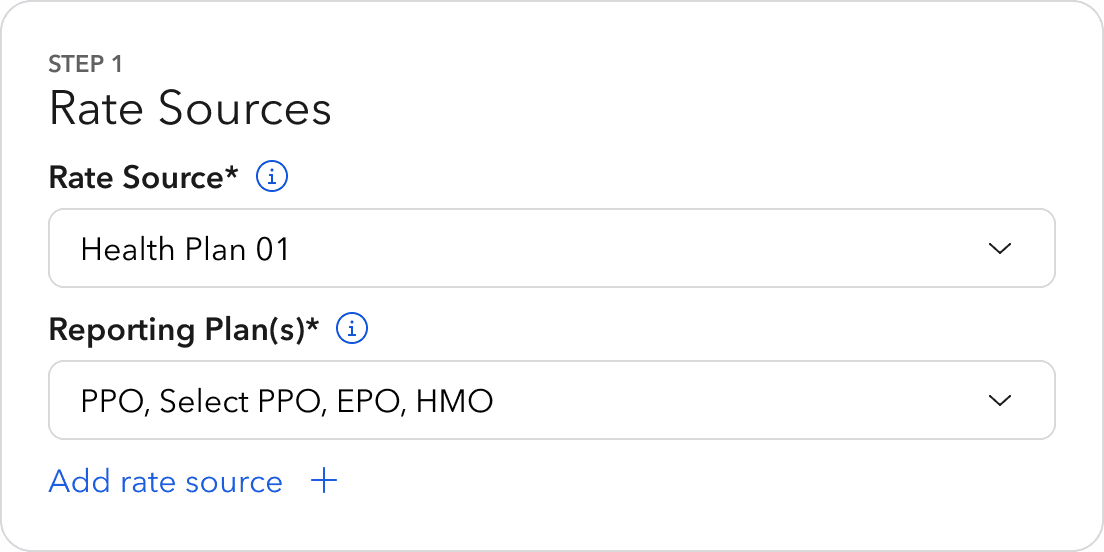
Speaking directly with plan administrators, we uncovered how users navigate rate negotiations and market insights to inform the granularity of analysis parameters.
Speaking directly with plan administrators, we uncovered how users navigate rate negotiations and market insights to inform the granularity of analysis parameters.
Speaking directly with plan administrators, we uncovered how users navigate rate negotiations and market insights to inform the granularity of analysis parameters.
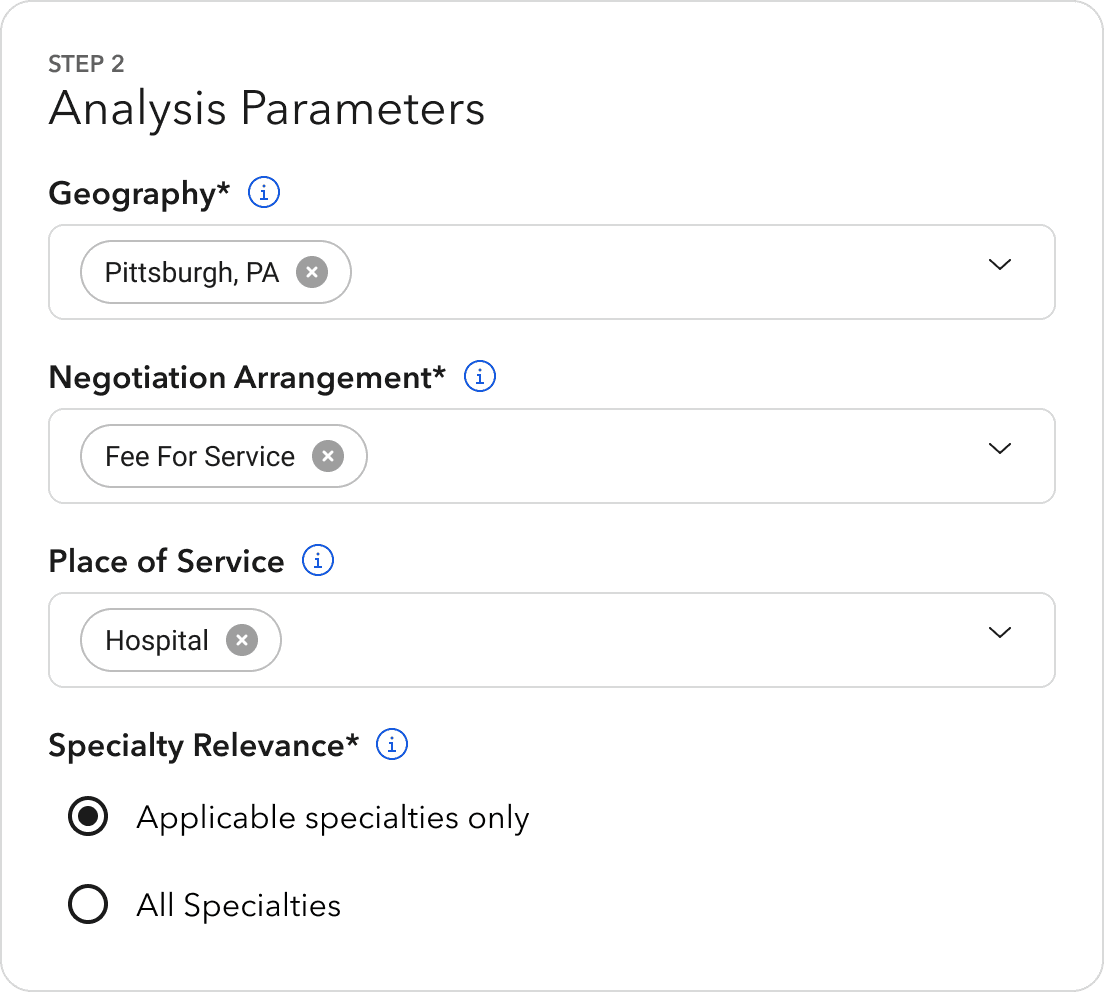
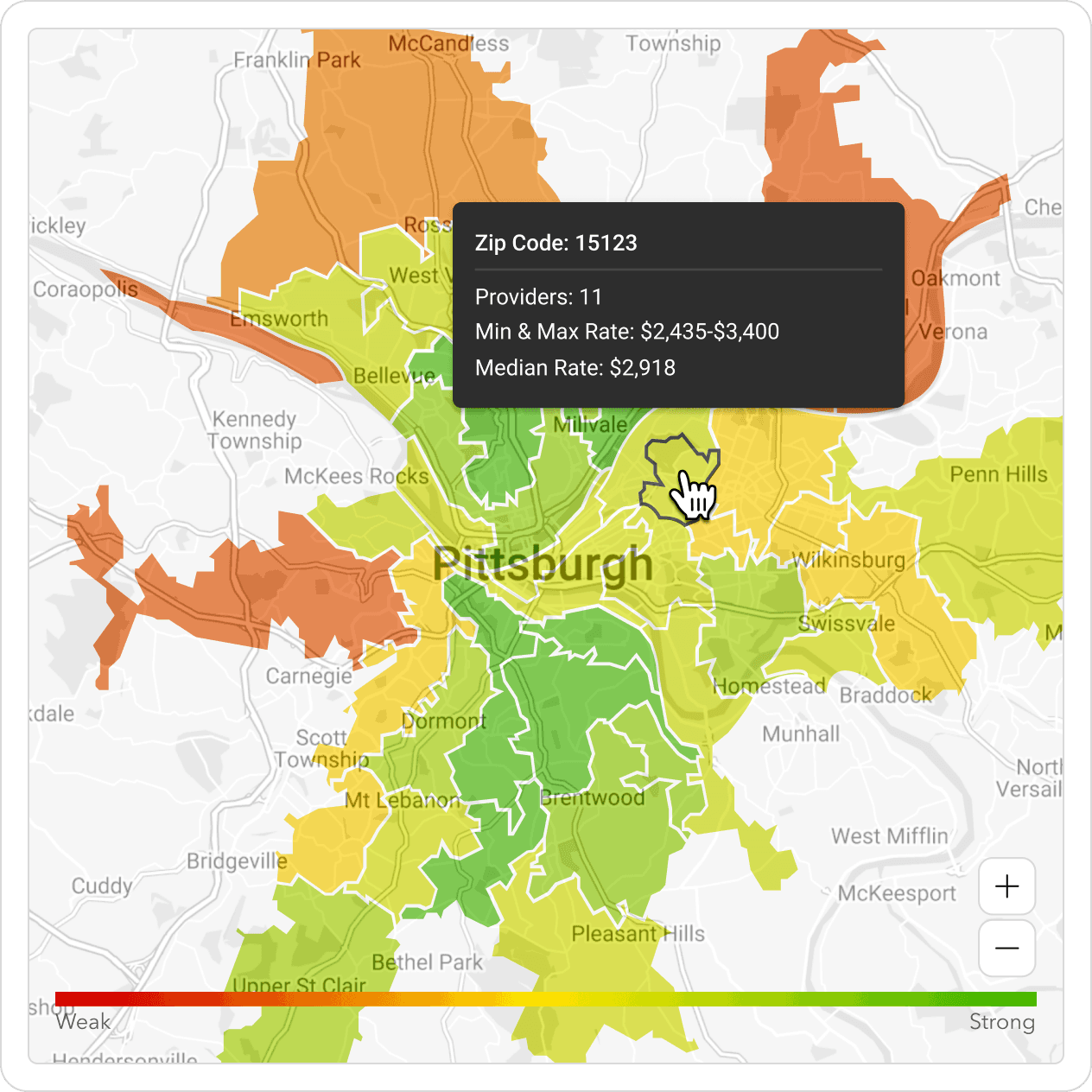
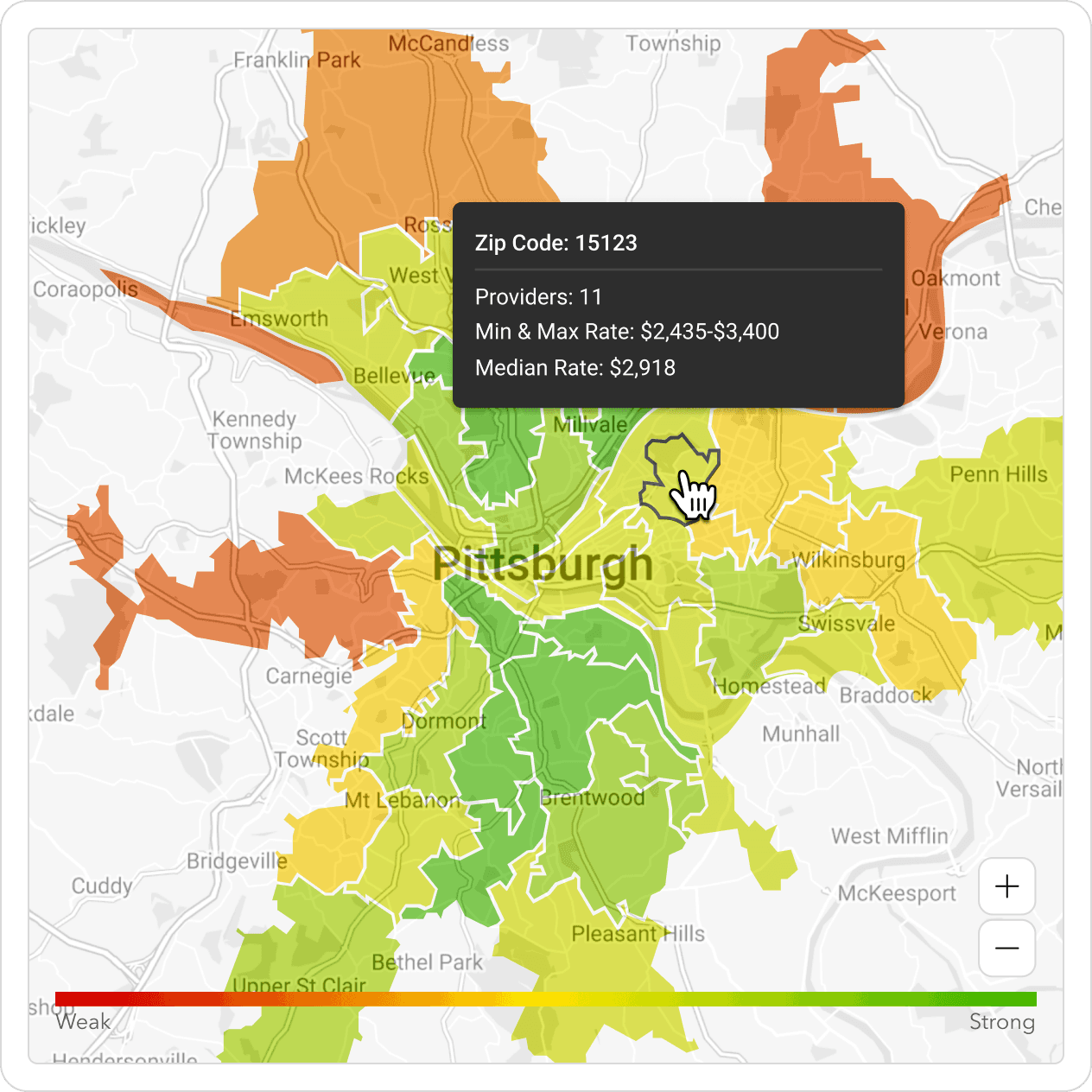
Geographic segmentation displays rich insights into the strength of a given provider network and portrays where competitor populations are being served.
Geographic segmentation displays rich insights into the strength of a given provider network and portrays where competitor populations are being served.
Geographic segmentation displays rich insights into the strength of a given provider network and portrays where competitor populations are being served.
/ Outcome
/ Outcome
/ Outcome
We effectively pioneered the first compliant product solution for health plans nationwide. This success led to Zelis's strategic acquisition of the Sapphire business, enabling growth to previously underserved markets.
We effectively pioneered the first compliant product solution for health plans nationwide. This success led to Zelis's strategic acquisition of the Sapphire business, enabling growth to previously underserved markets.
We effectively pioneered the first compliant product solution for health plans nationwide. This success led to Zelis's strategic acquisition of the Sapphire business, enabling growth to previously underserved markets.
/ Reflection
/ Reflection
/ Reflection
Medical rate data is unstandardized, infrequently updated, and often inaccurate, which deteriorates the effectiveness of this tool. Until the Transparency in Coverage law is enforced, insurers will continue to delay providing satisfactory data.
Medical rate data is unstandardized, infrequently updated, and often inaccurate, which deteriorates the effectiveness of this tool. Until the Transparency in Coverage law is enforced, insurers will continue to delay providing satisfactory data.
Medical rate data is unstandardized, infrequently updated, and often inaccurate, which deteriorates the effectiveness of this tool. Until the Transparency in Coverage law is enforced, insurers will continue to delay providing satisfactory data.